Peptides

Last Updated
Jan 2, 2026
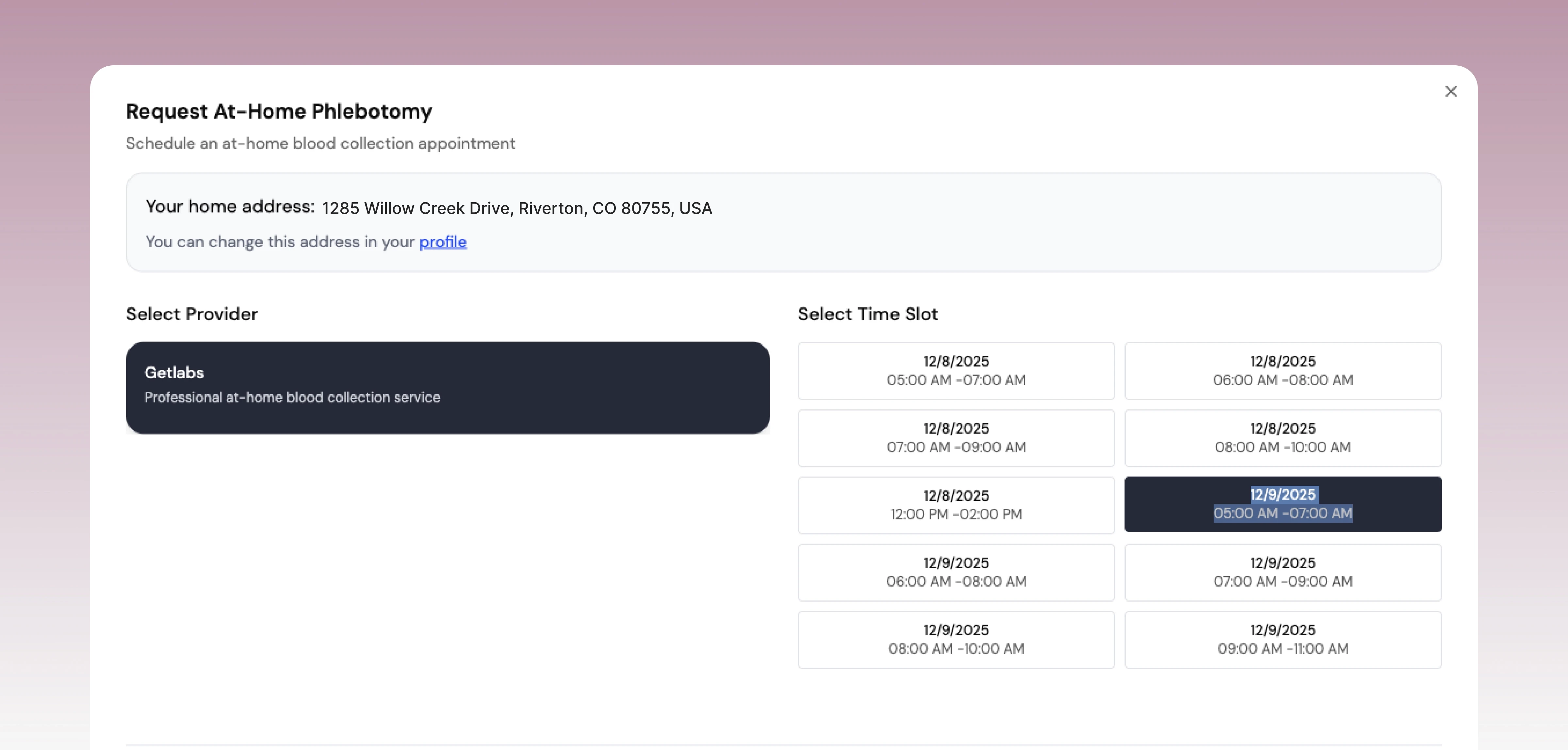
My journey into hormonal optimization began not with a dramatic health crisis, but with a slow, creeping decline in energy, focus, and overall vitality. I felt "off," and I suspected my testosterone levels were a key part of the puzzle. While Testosterone Replacement Therapy (TRT) is a well-known path, my personal research into more nuanced, targeted approaches led me deep into the world of peptide therapy. This exploration was about finding a way to work with my body's own systems, not just override them.
This article is the culmination of that personal investigation, guided by a commitment to professional, evidence-based health information. I wanted to find the best peptide for testosterone that could support the body's natural production pathways. Instead of a simple "one-size-fits-all" solution, I discovered a spectrum of powerful signaling molecules, each with a unique mechanism for influencing the hypothalamic-pituitary-gonadal (HPG) axis—the very command center for hormone production.
Here, we will break down the most relevant peptides for testosterone support, moving beyond the hype to provide a clear-eyed look at the science. We will explore:
The specific mechanism of each peptide.
The clinical context where each is most appropriately used.
Potential benefits and risks to consider.
How they compare to traditional TRT.
My goal is to provide a structured, actionable guide for anyone on a similar path. This is for the health-conscious individual who, like me, wants to leverage data, clinical guidance, and targeted therapies to reclaim their hormonal balance and optimize their performance. Let's get started.
1. GnRH (Gonadotropin-Releasing Hormone)
Gonadotropin-Releasing Hormone (GnRH) is the master regulator of your body's natural testosterone production system. Think of it as the very first domino in the chain reaction that leads to healthy testosterone levels. Produced in the hypothalamus, this peptide hormone signals the pituitary gland to release two other crucial hormones: Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). These hormones then travel to the testes, directly stimulating them to produce testosterone and maintain fertility.

Because it sits at the top of this entire hormonal cascade, known as the Hypothalamic-Pituitary-Gonadal (HPG) axis, GnRH represents a powerful and fundamental approach to optimizing testosterone. Using a synthetic form of GnRH is essentially a way to "reboot" or restore the body's own testosterone-making machinery, rather than replacing the final product with an external source like TRT. This makes it a potential best peptide for testosterone in specific clinical situations.
How GnRH Works: The Pulsatile Approach
The most critical aspect of GnRH function is its pulsatile nature. Your body releases it in short bursts, approximately every 90 to 120 minutes. This rhythmic pulse is essential for the pituitary to respond correctly. A continuous, non-pulsing stream of GnRH paradoxically shuts down LH and FSH production, a mechanism used in certain medical treatments to lower testosterone.
Therefore, therapeutic use of GnRH to boost testosterone requires mimicking this natural rhythm. This is typically achieved through a specialized micro-infusion pump that delivers a precise dose of a synthetic GnRH analogue (like gonadorelin) subcutaneously at regular intervals.
Key Insight: The success of GnRH therapy hinges on replicating the body's natural, rhythmic release. It is not a simple injection but a sophisticated, biomimetic process that restores the entire HPG axis from the top down.
Clinical Context and Ideal Candidate
So, when is this complex therapy the right choice? GnRH is primarily used for men diagnosed with secondary hypogonadism, specifically a condition called isolated hypogonadotropic hypogonadism (IHH). This means the testes are healthy and capable of producing testosterone, but the signal from the brain (the hypothalamus and pituitary) is absent or insufficient.
Primary Use Case: Restoring testosterone production and fertility in men with IHH.
Benefits: Unlike TRT, which suppresses the body's own production, pulsatile GnRH therapy kickstarts it. This maintains testicular size, function, and sperm production.
Comparison to hCG: While hCG (human chorionic gonadotropin) also stimulates the testes, it bypasses the brain and pituitary. GnRH works further upstream, restoring the entire axis for a more comprehensive physiological effect.
Implementation and Monitoring
Administering GnRH is a medically supervised process that demands precision and commitment. It is not a therapy for self-administration or casual experimentation.
Actionable Tips for Patients:
Find a Specialist: This therapy must be managed by an endocrinologist with experience in reproductive health and pulsatile hormone administration.
Commit to the Pump: You will need to wear a portable infusion pump programmed to deliver pulses of GnRH every 90-120 minutes. Consistency is non-negotiable for success.
Rigorous Monitoring: Expect frequent blood tests to track LH, FSH, and testosterone levels. Your clinician will adjust the pump's dosage and frequency based on these lab results and your body's response.
Patience is Key: It can take several months to fully normalize hormone levels and see the full benefits, which range from improved energy and libido to restored fertility.
2. HCG (Human Chorionic Gonadotropin)
Human Chorionic Gonadotropin (HCG) is a powerful peptide hormone that acts as a direct stimulant for your body's testosterone factories. It functions by mimicking Luteinizing Hormone (LH), one of the key signals sent from the pituitary gland. When HCG is introduced, it binds to the LH receptors on the Leydig cells within the testes, commanding them to produce testosterone and maintain testicular volume.
Unlike GnRH which works from the top of the hormonal cascade, HCG bypasses the brain and pituitary altogether. It delivers its message straight to the source, making it a highly effective and predictable tool for boosting endogenous testosterone production. This direct action makes it arguably the best peptide for testosterone in scenarios where the testes are healthy but need a direct "on" signal, such as during or alongside Testosterone Replacement Therapy (TRT).
How HCG Works: Direct Testicular Stimulation
The mechanism of HCG is straightforward and potent. While your brain is the CEO (hypothalamus) and the pituitary is the manager, HCG goes right to the factory floor (the testes) and tells the workers (Leydig cells) to get to work. This direct stimulation offers a reliable way to increase testosterone levels without relying on the complex signaling of the HPG axis.
Because it directly mimics LH, HCG can prevent the testicular atrophy and shutdown of natural testosterone synthesis that often occurs with standalone TRT. By keeping the testes active and functional, it preserves fertility and a more holistic hormonal balance, which is why it's a staple in many modern hormone optimization protocols. For a deeper dive into how this fits into a comprehensive strategy, you can learn more about optimizing your testosterone levels.
Clinical Context and Ideal Candidate
HCG's unique mechanism makes it suitable for very specific clinical situations, often as a complementary therapy rather than a standalone solution for low testosterone.
Primary Use Case: Preventing testicular atrophy and maintaining fertility for men on Testosterone Replacement Therapy (TRT).
Secondary Use Case: Used in fertility clinics to restart testosterone and sperm production in men with secondary hypogonadism before assisted reproduction.
Off-Label Use: Employed as part of a "post-cycle therapy" (PCT) protocol in performance enhancement communities to help restore natural testosterone production after a cycle of anabolic steroids.
Implementation and Monitoring
Administering HCG requires medical supervision to ensure proper dosing and to manage potential side effects like elevated estrogen. It is a powerful tool that should not be used without clinician guidance.
Actionable Tips for Patients:
Work with a Knowledgeable Clinician: Seek a physician specializing in hormone replacement therapy who understands the nuances of HCG dosing and monitoring.
Standard Dosing Protocols: Typical doses range from 500-1000 IU, administered 2 to 3 times per week via subcutaneous injection. This mimics a more stable physiological signal.
Monitor Estrogen Levels: Stimulating testosterone production can also increase its conversion to estrogen. Your clinician will monitor estradiol levels and may prescribe an aromatase inhibitor if they become elevated.
Expect Timely Results: The effects of HCG are relatively quick. Most men notice improvements in testicular volume and well-being within 2 to 4 weeks of starting therapy.
3. Kisspeptin (Kiss1)
Kisspeptin is a powerful neuroendocrine peptide that acts as a "master switch" for the reproductive system, operating even one level above GnRH. Think of it as the conductor who cues the first domino in the hormonal orchestra. Produced in the hypothalamus, kisspeptin directly activates the GnRH-producing neurons, triggering the entire cascade that leads to the pituitary releasing LH and FSH, and ultimately, testosterone production in the testes.
Because it functions at the very genesis of the HPG axis, kisspeptin represents a cutting-edge approach to diagnosing and potentially treating low testosterone. Instead of replacing the end hormone or even stimulating the pituitary, kisspeptin therapy aims to restore the primary neural signal itself. This makes it an incredibly promising candidate as a best peptide for testosterone, particularly for understanding and treating complex cases of hypogonadism.
How Kisspeptin Works: The Neural Activator
The primary role of Kisspeptin is to stimulate GnRH neurons, which are responsible for the pulsatile release of GnRH. This makes it a fundamental regulator of the entire reproductive hormonal system. Its action is so potent that it has been studied as a tool to kick-start puberty in delayed cases and to treat hormonal disorders stemming from faulty signaling in the brain.
Administering kisspeptin can lead to a robust and immediate increase in GnRH, LH, FSH, and subsequently, testosterone. This provides a direct way to test whether the entire HPG axis is functional from the brain all the way down to the testes, offering unique diagnostic insights that other methods cannot.
Clinical Context and Ideal Candidate
Currently, kisspeptin is primarily used in clinical research and advanced diagnostic settings, not as a mainstream therapy. Pioneering research, such as studies from Imperial College London, has explored its use in treating men with low libido and certain forms of hypogonadism. Its main application is for men with suspected central (or secondary) hypogonadism, where the issue lies within the hypothalamus or pituitary.
Primary Use Case: Investigational treatment and diagnosis for certain types of male infertility and hypogonadism.
Benefits: Offers a more natural restoration of the entire hormonal axis than direct testosterone replacement. It has also shown potential benefits for improving mood and libido, independent of its effect on testosterone.
Comparison to GnRH: While GnRH directly signals the pituitary, kisspeptin signals the GnRH neurons themselves. This makes it an even more "upstream" intervention, addressing the neural control of the entire system.
Implementation and Monitoring
Kisspeptin administration is strictly a medically supervised procedure confined to research trials and specialized endocrinology centers. It is not available for public use or self-administration and should not be sought from unregulated sources.
Actionable Tips for Patients:
Seek an Expert: If you have a complex case of hypogonadism, consult a reproductive endocrinologist at a major academic medical center, who may be aware of or involved in kisspeptin research.
Understand the Administration: In clinical trials, kisspeptin is often administered as an intravenous (IV) infusion or subcutaneous injection under strict medical observation to monitor its effects.
Expect Comprehensive Monitoring: This is an advanced intervention. Expect detailed and frequent blood work to measure LH, FSH, GnRH, testosterone, and other related hormones to gauge the HPG axis response.
View it as Investigational: Understand that kisspeptin therapy is still largely in the research phase. Its long-term safety and efficacy profile as a routine treatment for low testosterone is still being established.
4. LHRH Agonists (Leuprolide, Triptorelin, Goserelin)
LHRH (Luteinizing Hormone-Releasing Hormone) agonists, also known as GnRH agonists, are synthetic peptides that paradoxically offer a unique, albeit temporary, window for boosting testosterone. These compounds, such as leuprolide, triptorelin, and goserelin, are structurally similar to natural GnRH. They work by binding to and initially stimulating the GnRH receptors on the pituitary gland, leading to a significant, short-lived surge in LH, FSH, and consequently, testosterone.
However, this initial stimulation is their defining feature and also their limitation for testosterone optimization. Unlike the body's natural pulsatile release of GnRH, these agonists provide continuous stimulation. This constant signal quickly desensitizes and downregulates the pituitary receptors, ultimately shutting down the HPG axis and plummeting testosterone to castrate levels. While their primary clinical use is to suppress testosterone (e.g., in prostate cancer treatment), harnessing the initial "flare" effect is a highly specialized application.
How LHRH Agonists Work: The Flare-and-Suppress Mechanism
The mechanism of LHRH agonists is a two-phase process. It's crucial to understand both phases to see why their role in boosting testosterone is so specific and short-term.
Stimulation Phase (The "Flare"): Upon first administration, the agonist intensely stimulates the GnRH receptors. The pituitary responds by releasing a large bolus of LH and FSH, which in turn signals the testes to ramp up testosterone production. This flare typically lasts for about 7 to 14 days.
Suppression Phase (Downregulation): After the initial flare, the continuous presence of the agonist overwhelms the pituitary receptors. They become desensitized and retract from the cell surface. This effectively halts LH and FSH secretion, leading to a profound drop in testosterone production.
Clinical Context and Ideal Candidate
The application of LHRH agonists for increasing testosterone is extremely narrow and not a standard therapy for general low T. It is almost exclusively used in contexts where a controlled, temporary hormonal surge is desired for diagnostic or procedural reasons.
Primary Use Case: In reproductive medicine, an LHRH agonist might be used to trigger a final oocyte maturation in certain IVF protocols or to test pituitary reserve.
Benefits: The initial flare provides a powerful, predictable surge in endogenous hormones, which can be useful for specific, time-sensitive clinical interventions.
Comparison to hCG/GnRH: Unlike pulsatile GnRH, which aims to restore long-term function, or hCG, which provides sustained stimulation, LHRH agonists offer a "one and done" spike followed by shutdown. This makes them unsuitable for ongoing testosterone optimization.
Implementation and Monitoring
Using an LHRH agonist for any purpose, especially one that manipulates the HPG axis, is a procedure reserved for specialists and is absolutely not a therapy for self-management or performance enhancement.
Actionable Tips for Patients:
Consult a Specialist: This approach should only ever be considered under the strict guidance of a reproductive endocrinologist or a urologist within a specific treatment protocol.
Understand the Timeline: Be fully aware that any testosterone increase is temporary and will be followed by a significant decrease. The therapeutic goal is not the testosterone boost itself but a different downstream effect.
Intensive Monitoring: Expect blood tests before, during, and after the flare period to precisely measure LH, FSH, and total/free testosterone levels. Understanding these values is crucial, and you can learn more about the free androgen index on Outlive.bio.
Plan for the Aftermath: A clear medical plan must be in place to manage the subsequent hormonal suppression, which is the intended long-term effect of these peptides.
5. PT-141 (Bremelanotide)
PT-141, known clinically as Bremelanotide, takes a unique and indirect route to supporting the ecosystem around healthy testosterone. Instead of directly stimulating hormone production, it primarily targets the central nervous system to enhance sexual arousal and function. Developed from the peptide hormone Melanotan II, PT-141 is a melanocortin receptor agonist, meaning it activates specific pathways in the brain associated with sexual desire and performance.
While its FDA-approved use (under the brand name Vyleesi) is for hypoactive sexual desire disorder in premenopausal women, it has gained significant off-label popularity for men. The connection to testosterone is rooted in the powerful link between libido, sexual activity, and hormonal health. By improving sexual function and desire, PT-141 can help reinforce the positive feedback loops that support the Hypothalamic-Pituitary-Gonadal (HPG) axis, making it a compelling candidate for the best peptide for testosterone in a supportive role.
How PT-141 Works: A Central Nervous System Approach
Unlike peptides that directly signal the testes or pituitary gland, PT-141 works centrally. It selectively binds to melanocortin receptors (specifically MC3-R and MC4-R) in the hypothalamus, a region of the brain that governs everything from appetite to sexual behavior. This activation bypasses the common vascular pathways targeted by drugs like Viagra and Cialis, instead initiating arousal directly from the brain.
This central mechanism is what makes PT-141 so intriguing. A healthy libido and regular sexual activity are known to correlate with more stable and robust testosterone levels. By restoring or enhancing this fundamental aspect of male health, PT-141 helps create an environment where the body's natural testosterone production can thrive.
Clinical Context and Ideal Candidate
PT-141 is best suited for men experiencing a disconnect between physical ability and mental desire, or those whose low libido is impacting their quality of life, even if their testosterone levels are within a normal range. It is often used as an adjunct therapy to address the psychological and neurological components of sexual health.
Primary Use Case: Addressing low libido, psychological erectile dysfunction, or enhancing sexual experience.
Benefits: Works on-demand, targets the root of desire in the brain, and can be effective when other ED medications fail. It can restore confidence and intimacy, which are crucial for overall well-being.
Comparison to TRT: While TRT raises baseline testosterone, it doesn't always translate to increased libido for everyone. PT-141 can be used alongside TRT to specifically target and amplify sexual desire, offering a more complete solution.
Implementation and Monitoring
Administering PT-141 is relatively straightforward but requires careful dosing and medical oversight to manage potential side effects. It is typically self-administered via a subcutaneous injection.
Actionable Tips for Patients:
Consult a Specialist: Discuss using PT-141 with a clinician in sexual medicine or a hormone optimization clinic to ensure it’s appropriate for your health profile.
Start with a Test Dose: Begin with a lower dose to assess your individual response and sensitivity, particularly regarding side effects like nausea or flushing.
Timing is Everything: For best results, administer the injection approximately 30-45 minutes before anticipated sexual activity. Effects can last for several hours.
Monitor Blood Pressure: PT-141 can cause a temporary increase in blood pressure. It's crucial to monitor this, especially if you have pre-existing cardiovascular concerns.
Use As-Needed: This is not a daily peptide. It is designed for on-demand use to avoid receptor desensitization and minimize side effects.
The Path Forward: Data, a Doctor, and a Personalized Plan
Navigating the complex landscape of hormonal health can feel overwhelming. This brief guide has explored several powerful compounds, from direct hormonal analogs like HCG to upstream regulators like Kisspeptin and GnRH, each with a unique mechanism for potentially influencing testosterone levels.
The central takeaway is this: there is no single "best peptide for testosterone" that applies universally. The most effective approach is not found in a vial but in a process. It’s a personalized strategy built on three pillars: objective data, expert medical guidance, and a plan tailored to your unique biology. The right peptide for a 35-year-old athlete seeking performance optimization will likely differ from the ideal choice for a 50-year-old experiencing symptoms of andropause.
Key Takeaways: From Information to Action
As you move forward, keep these core principles in mind to make informed, safe, and effective decisions about your hormonal health:
Mechanism Matters Most: Understanding how a peptide works is critical. Does it directly mimic a hormone (like HCG) or act at the hypothalamus (like Kisspeptin)? This distinction determines its suitability and the necessary monitoring protocol.
Data is Your Compass: You cannot manage what you do not measure. Establishing a baseline through comprehensive lab work (Total T, Free T, SHBG, LH, FSH, Estradiol) is non-negotiable. Ongoing monitoring provides the feedback loop needed to assess efficacy and adjust protocols safely.
Expert Supervision is Mandatory: This is not a do-it-yourself endeavor. The potential for disrupting your entire endocrine system is significant. Working with a qualified physician is the only responsible way to explore peptide therapies. They can interpret your lab results, design a safe protocol, and manage any side effects. You can learn how to read blood work results for beginners as a key part of this process.
Your Next Steps: Building a Personalized Protocol
Ready to translate this knowledge into a concrete plan? Here’s a step-by-step guide to taking control of your hormonal health.
Quantify Your Baseline: Before considering any intervention, get a clear picture of where you stand. Schedule comprehensive blood work to assess your full hormonal panel.
Consult with a Specialist: Find a medical professional who specializes in hormone optimization and peptide therapies. Bring your lab results to your consultation for a data-driven discussion.
Define Your Goals: Be specific. Are you trying to resolve symptoms of low T, or are you aiming to optimize your levels for better athletic performance?
Commit to a Monitored Protocol: If you and your doctor decide a peptide protocol is the right fit, commit to the process. This includes adhering to the prescribed dosing schedule and following up with periodic lab tests.
Ultimately, mastering your hormonal health is a journey of personalized medicine. The search for the "best peptide for testosterone" evolves into a more sophisticated question: "What is the best, data-informed, and medically supervised strategy for my specific hormonal needs?" By embracing this mindset, you shift from chasing a magic bullet to building a sustainable system for long-term vitality and performance.
Navigating this intricate process requires a partner dedicated to data-driven, personalized health. Outlive Biology specializes in creating comprehensive, clinician-supervised plans that integrate advanced lab testing, wearable data, and targeted therapies like TRT to optimize your hormones. If you're ready to move beyond generic advice and build a protocol tailored to your unique biology, explore how we can help at Outlive Biology.

Live better for longer.
Research-backed tools, tactics, and techniques to maximize your health, delivered to your inbox every Monday.
Because real transformation starts with trust
and trust starts with clarity.
Founding Member Discount
Includes Devices + Labs
Cancel Anytime Before Activation