Hormones

Last Updated
Jan 2, 2026
Estradiol levels are a huge piece of the puzzle when it comes to a woman's reproductive health and overall well-being. During your reproductive years, levels can swing anywhere from 30 to 400 pg/mL, but they drop to less than 30 pg/mL after menopause. This isn't just a number—it’s a direct reflection of a hormone that acts like a master switch for everything from your menstrual cycle to your bone density and even your mood.
Getting a handle on what your estradiol levels are doing is a crucial first step in taking control of your health.
What Is Estradiol and Why Does It Matter?
If your body's hormonal system were an orchestra, estradiol would be the conductor. It's the most powerful and prominent form of estrogen working in your body during your reproductive years, and its job goes way beyond fertility. While it's mainly produced in the follicles of your ovaries, smaller amounts also come from your adrenal glands and fat cells.
Estradiol’s most famous role, of course, is running the show for the menstrual cycle. Its predictable rise and fall are the signals that tell your body to prepare for ovulation and a potential pregnancy. But that's just the beginning of the story.
The Conductor of Female Physiology
Think of estradiol as a key that fits into locks all over your body. It’s not just about periods; it’s about keeping your entire system running smoothly. This one little molecule is responsible for building up and maintaining the health of so many different tissues.
That’s why tracking estradiol is so important for getting a full picture of your health. When the conductor is on point, the whole orchestra sounds amazing. But if the timing is off—if estradiol is too high or too low—the whole symphony can start to sound chaotic, and you’ll feel the effects every single day.
Estradiol is so much more than a reproductive hormone. It’s a critical messenger that’s essential for keeping your skeleton, heart, and brain healthy. The sharp decline during menopause is linked to a higher risk for several chronic diseases, which really underscores its lifelong importance.
Core Functions Directed by Estradiol
You can feel the impact of estradiol from head to toe. From your brain to your bones, it plays a vital and protective role. Here are some of its most important jobs:
Regulating the Menstrual Cycle: The mid-cycle surge of estradiol is what actually triggers ovulation—the release of an egg from the ovary. It's the main event of your cycle.
Supporting Bone Density: Estradiol keeps your bones strong by managing the natural process of bone breakdown and rebuilding. This is why bone loss can speed up dramatically after menopause when estradiol levels plummet.
Promoting Cardiovascular Health: It helps keep cholesterol in a healthy range and ensures your blood vessels stay flexible, which gives your heart a bit of a protective shield.
Influencing Mood and Cognition: Estradiol has a huge effect on brain chemicals like serotonin, which can impact everything from your mood and memory to your ability to focus.
Knowing what estradiol does makes it much easier to understand why shifts in its levels—whether from your monthly cycle, perimenopause, or another health issue—can make you feel so different. It’s the starting point for being proactive about your hormonal health.
What Are Normal Estradi-ol Levels?
Trying to pin down a single "normal" number for estradiol is a bit like trying to describe "normal" weather—it completely depends on the season of your life. Your hormonal landscape is anything but static. Instead, estradiol levels in women are designed to shift in a predictable, rhythmic pattern from puberty all the way through menopause.
These fluctuations aren't random; they're the very engine driving your body’s major transitions. A level that's perfectly healthy during ovulation would be a major red flag after menopause. To make sense of your own health, you first have to understand this journey.
The image below hints at just how far-reaching estradiol's job description is, covering everything from managing your menstrual cycle to keeping your bones strong and your mind sharp.

As you can see, estradiol's influence goes far beyond just reproduction. It’s a key player in your overall health and well-being.
Estradiol During Your Reproductive Years
Throughout your reproductive years, estradiol acts like the lead dancer in a beautifully choreographed performance, with levels rising and falling throughout your menstrual cycle. We can break this monthly rhythm down into a few distinct acts.
First up is the follicular phase, which kicks off on day one of your period. At the very beginning, estradiol is at its lowest. But as your ovaries get busy preparing an egg for release, follicles start to mature and churn out more and more estradiol. This ramp-up is what thickens your uterine lining, getting it ready for a potential pregnancy.
This predictable rise and fall is exactly why a single estradiol test without context can be so misleading. A good clinician will always ask where you are in your cycle to interpret the results correctly.
Next is the ovulatory phase, a brief but crucial window. Estradiol surges to its highest peak of the entire month—a dramatic spike that tells your brain it's time to release luteinizing hormone (LH). That LH surge is the final trigger that causes the dominant follicle to release its egg.
Finally, the cycle winds down with the luteal phase. After ovulation, estradiol takes a quick dip before rising again for a second, more sustained peak. This helps maintain the uterine lining just in case. If pregnancy doesn't happen, both estradiol and progesterone levels plummet, signaling your period to start and kicking off a brand new cycle.
Puberty, Perimenopause, and Menopause
Estradiol levels don't just change month to month; they undergo massive shifts across your entire lifespan. Before puberty, levels are practically nonexistent. But as puberty starts, the ovaries "wake up" and begin producing estradiol, which drives the development of secondary sex characteristics like breast growth and the start of menstruation.
The transition toward menopause, known as perimenopause, is famous for its hormonal chaos. Often starting in a woman's 40s, this phase is defined by erratic and unpredictable estradiol swings. Ovarian function is declining, but it's not a smooth, straight line down. One month your levels might be sky-high, and the next they could be in the basement, leading to irregular cycles and classic symptoms like hot flashes and mood swings.
Eventually, you reach menopause, which is officially marked by twelve consecutive months without a period. By this point, your ovaries have largely retired from estradiol production. Levels drop dramatically and settle at a new, much lower baseline. While normal estradiol for a premenopausal woman can range from 30 to 400 pg/mL, postmenopausal levels typically fall to between 0 and 30 pg/mL. You can learn more about these reference ranges for estrogen and its various roles.
This steep decline is what drives many menopausal symptoms and increases the risk for health issues like osteoporosis, making hormonal awareness more important than ever during this stage of life.
Reference Ranges for Estradiol Levels in Women
The table below provides a snapshot of typical serum estradiol levels according to different life stages and phases of the menstrual cycle. It's important to remember that these are general guidelines—individual results and lab ranges can vary.
Life Stage / Cycle Phase | Typical Range (pg/mL) | Typical Range (pmol/L) |
|---|---|---|
Puberty (Tanner Stage II-III) | <30 pg/mL | <110 pmol/L |
Follicular Phase | 20 - 150 pg/mL | 73 - 551 pmol/L |
Ovulatory Peak | 40 - 350 pg/mL | 147 - 1285 pmol/L |
Luteal Phase | 30 - 250 pg/mL | 110 - 918 pmol/L |
Perimenopause | Highly variable, often fluctuating wildly | Highly variable |
Post-menopause | <30 pg/mL | <110 pmol/L |
As the data shows, what's "normal" is entirely dependent on context. A level of 150 pg/mL could be perfectly healthy during ovulation but would be unusual during the early follicular phase or after menopause.
Recognizing the Signs of High Estradiol
Think of your hormones as a complex chemical conversation. When everything is balanced, the conversation flows smoothly. But when estradiol levels get too high, it's like one voice shouting over everyone else. This situation, often called estrogen dominance, happens when estradiol is out of proportion with its counterpart, progesterone.
This isn't just a number on a lab report; it’s an imbalance that throws your body's natural rhythm out of sync, leading to a cascade of frustrating physical and emotional symptoms. Understanding what might be causing this shift is the first step toward getting things back on track.

Recognizing the patterns of estrogen dominance is key. It gives you the information you need to have a productive conversation with your healthcare provider and start looking for solutions.
Common Causes of Elevated Estradiol
High estradiol doesn't just happen randomly. It's almost always a downstream effect of other factors that are either cranking up estrogen production or, just as importantly, getting in the way of your body’s ability to clear it out.
Here are some of the usual suspects:
Medical Conditions: A classic example is Polycystic Ovary Syndrome (PCOS), which can disrupt the entire hormonal cascade and lead to elevated estrogen. In much rarer cases, certain ovarian tumors can also secrete excess estradiol.
Body Composition: Fat tissue isn't just inert storage; it’s metabolically active and can produce its own estrogen. So, higher levels of body fat can directly contribute to a higher overall estradiol load.
Sluggish Liver Function: Your liver is the primary detox organ, responsible for breaking down used-up hormones. If it's overworked or impaired, it can't metabolize estradiol efficiently, allowing levels to creep up.
Medications: Some forms of hormone replacement therapy (HRT), if not dosed or monitored carefully, can easily push estradiol levels into an uncomfortably high range.
Often, it's not just one of these things but a combination of factors that creates the perfect storm for estrogen dominance.
Physical Symptoms of High Estradiol
When estradiol is running the show, the physical signs are often the first things you'll notice. These symptoms can feel relentless and often get worse during the second half of your menstrual cycle, as progesterone is supposed to be rising but can't keep up.
Think of it this way: high estradiol keeps your body in a constant "build-up" phase without progesterone's calming, balancing influence. This leads to overstimulation of tissues in the breasts and uterus, which is where many of the most common complaints come from.
Keep an eye out for these patterns:
Persistent Bloating and Water Retention: A constant feeling of puffiness, especially in your abdomen, hands, and feet, that doesn't seem to go away.
Breast Tenderness or Swelling: Your breasts might feel heavy, sore, or lumpy—sometimes referred to as fibrocystic breasts.
Heavy or Irregular Periods: High estradiol can cause the uterine lining to over-thicken, leading to extremely heavy bleeding (menorrhagia) or unpredictable cycles.
Weight Gain (Especially Hips & Thighs): Estradiol influences where your body stores fat. When it's too high, it can make it stubbornly difficult to lose weight from the hips, thighs, and butt.
Worsening PMS: If your premenstrual symptoms feel more severe than just typical discomfort, it can be a major clue that your hormones are out of balance.
Emotional and Cognitive Signs
The effects of high estradiol aren't just physical. This powerful hormone has a direct line to your brain, influencing key neurotransmitters like serotonin and dopamine that regulate your mood. When estradiol is too high, your mental and emotional state can take a real hit.
These shifts can be just as disruptive as the physical symptoms, with many women reporting they just don't feel like themselves. Pay attention to changes in your mental state, such as:
Mood Swings and Irritability
Increased Anxiety or Panic Feelings
Brain Fog or Trouble Concentrating
Persistent Fatigue or Low Energy
Headaches or Migraines, Especially Cyclical Ones
The goal here isn't to self-diagnose. It's about gathering clues. These are the data points you can bring to your doctor to start an informed investigation into what's really going on with your hormonal health.
What Does Low Estradiol Feel Like?
When your body doesn't have enough estradiol, things can start to feel... off. Think of estradiol as a master regulator—when it's in short supply, a lot of different systems can get thrown out of whack. This is the defining experience of perimenopause and menopause, but it’s not just an age-related issue.
Sometimes, factors like intense endurance training, maintaining a very low body weight, or even problems with the pituitary gland can cause estradiol to drop, regardless of your age. No matter the reason, the symptoms can be physically and mentally draining, leaving you feeling like you're running on empty.
Physical Signs: From Classic to Surprising
The most famous signs of low estradiol are the ones that mess with your internal thermostat. These "vasomotor symptoms" are often the first red flags that your hormone levels are shifting.
Hot Flashes: That sudden, creeping wave of intense heat that rushes over your face and upper body.
Night Sweats: Hot flashes that crash your sleep party, leaving you and your sheets soaked.
But the effects of low estradiol run much deeper than just temperature. Many women are caught off guard when they learn that other nagging issues are tied directly to this hormonal dip. For example, unexpected joint pain can crop up because estradiol helps keep inflammation in check. A persistent, bone-deep fatigue can also take hold, making even simple daily activities feel like a huge effort.
Low estradiol doesn't just make you tired; it fundamentally changes your body's risk profile. When estradiol drops, it leaves tissues like bones and blood vessels more vulnerable, altering long-term health in significant ways.
Brain Fog, Mood, and Beyond
Estradiol’s influence extends right into your brain, where it helps regulate the neurotransmitters that control your mood, memory, and focus. When your levels are low, it's common to feel like you're navigating a constant mental haze.
Many women describe this as brain fog—that frustrating feeling of being a step behind, struggling to find the right word or concentrate on a task. At the same time, new or worsening feelings of anxiety can surface, often without a clear trigger. These aren't just you "being emotional"; they are a direct physiological response to your brain getting fewer signals from its key estrogen.
After menopause, estradiol levels can plummet, often settling under 30 pg/mL. This dramatic drop isn't just about symptoms; it's linked to a higher risk for serious health problems like cardiovascular disease and osteoporosis. A 2023 study, for instance, confirmed that lower circulating estrogen in menopausal women is tied to a greater risk of heart-related events. You can explore more research on how estrogen levels impact long-term health on Science.gov(http://Science.gov). Recognizing and validating these symptoms is the first, most important step toward getting the right support.
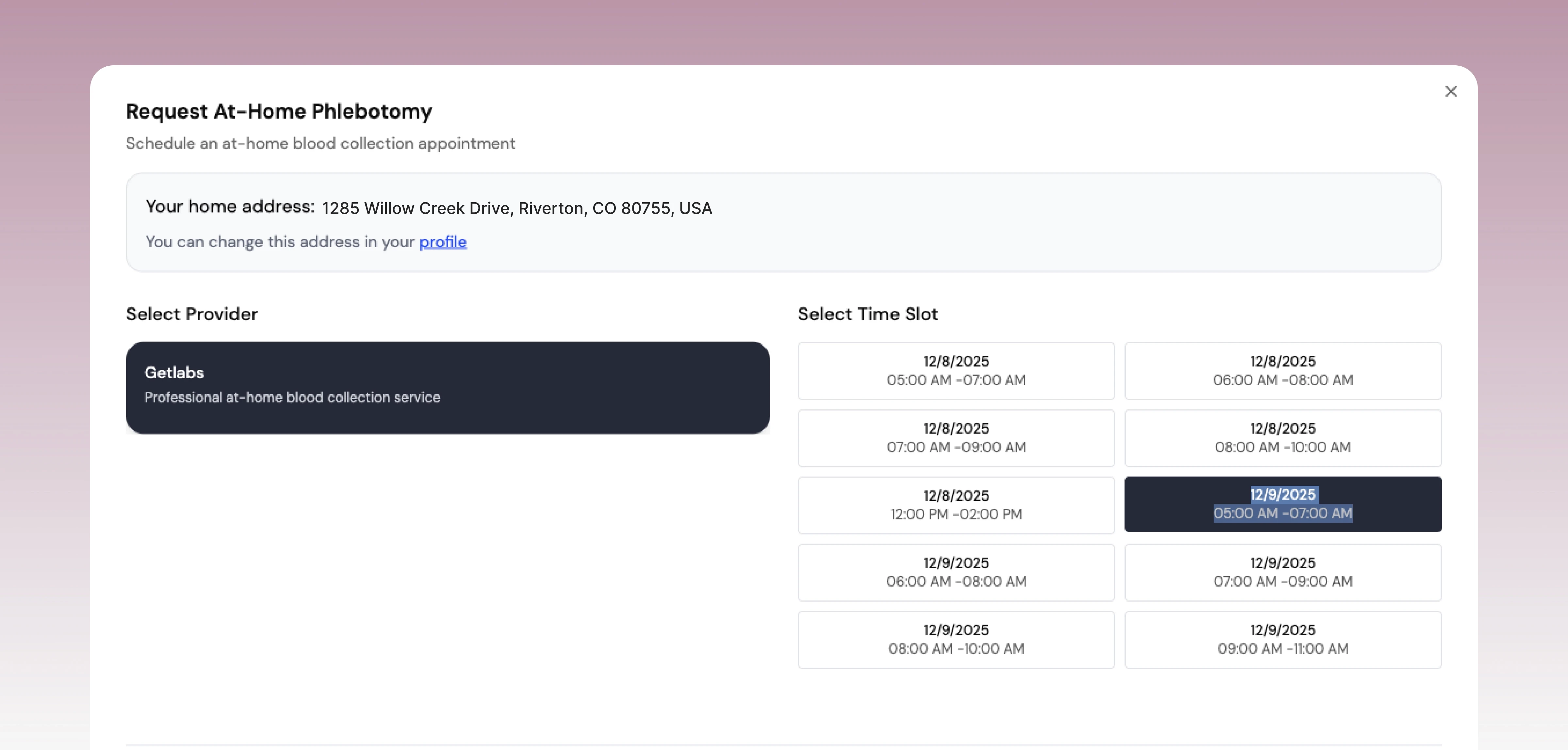
How to Properly Test Your Estradiol Levels
Figuring out your estradiol levels isn't as simple as getting a one-off blood draw. Since this hormone ebbs and flows dramatically throughout your menstrual cycle, a single test is just a snapshot in time—it doesn't tell the whole story. To get a clear and clinically useful picture, you have to be strategic about the process, considering timing, the type of test, and what other hormones are being measured alongside it.
This isn't about playing doctor at home; it’s about using lab testing as a powerful tool in partnership with your healthcare provider. A properly timed and interpreted test can bring immense clarity, while a poorly timed one can create more confusion than it solves.
Why Timing Is Everything
For women who are still menstruating, timing is absolutely crucial for an accurate reading. Think of your menstrual cycle as a 28-day narrative with a distinct beginning, middle, and end. Testing on the wrong "day" of that story gives you a result completely devoid of context.
The most common—and most valuable—time to test is on Day 3 of your cycle, with Day 1 being the first day of your period. This is early in the follicular phase when estradiol and other key hormones are at their baseline. Testing at this specific point provides a stable, reliable starting point that helps clinicians assess your fundamental ovarian function.
Context is king. An estradiol level of 150 pg/mL on Day 3 would raise a red flag, but that very same number would be perfectly normal around ovulation. Without the context of timing, the number itself is almost meaningless.
The Hormone Panel: Seeing the Full Picture
Estradiol doesn't act alone. It’s part of a complex hormonal orchestra, and to truly understand what your levels mean, clinicians almost always measure it as part of a broader hormone panel. This allows them to see how it interacts with the other key players.
Two of the most important companion hormones are:
Follicle-Stimulating Hormone (FSH): This hormone, made in your pituitary gland, is the one that tells your ovaries to start preparing an egg. On Day 3, high FSH paired with low estradiol can suggest diminishing ovarian reserve.
Luteinizing Hormone (LH): Another pituitary hormone, LH is the one that surges mid-cycle to trigger ovulation. The ratio of LH to FSH is also a key diagnostic clue, especially for conditions like PCOS.
Looking at these hormones together allows your doctor to see the full conversation happening between your brain and your ovaries. A full picture often includes other markers, which is why labs are so useful. You can learn more about how labs provide a wider view of your health in our guide on the comprehensive metabolic panel.
Choosing the Right Test
While a few methods exist for measuring hormones, they are not all created equal when it comes to clinical reliability for estradiol.
Serum (Blood) Test: This is the gold standard, no question. A blood sample drawn from a vein provides the most accurate and widely accepted measurement of the estradiol actually circulating in your system.
Saliva Test: Though convenient, saliva tests can be less reliable. Hormone concentrations in saliva are easily influenced by collection methods and don't always reflect what's happening in your bloodstream.
Urine Test: This method is often used in fertility tracking to detect hormone metabolites (like byproducts of estrogen and LH). A 24-hour urine collection can give an average over a day, but for a precise diagnostic measurement, a serum test is always preferred.
A Note on Perimenopause: Testing during the perimenopausal transition is notoriously tricky. Your hormones can fluctuate so erratically that one day's results might look completely different from the next. This makes it incredibly challenging to use a single blood test to diagnose this phase of life.
In fact, because of the wild variability and the influence of factors like hormone therapy, blood testing is often considered an unreliable sole marker for diagnosing perimenopause. Clinical decisions have to include a broader physiological context and symptom tracking. For this reason, many clinicians will diagnose perimenopause based on symptoms, age, and cycle changes rather than a single lab value.
Actionable Steps for Supporting Hormone Balance
Knowing your estradiol number is a great first step, but the real magic happens when you turn that knowledge into daily action. While medical treatments definitely have their place, you can't overlook the powerful foundation of nutrition, exercise, stress management, and sleep.
Think of these lifestyle habits as the bedrock for hormonal health. They create an environment where your body’s intricate hormonal symphony can play in tune.
Fuel Your Body for Hormonal Harmony
The food on your plate provides the literal building blocks for your hormones. A diet centered around nutrient-packed whole foods is non-negotiable for maintaining stable estradiol levels in women.
Try to build your meals around a few key components:
Fiber is Your Friend: Getting enough fiber from leafy greens, beans, and whole grains is a game-changer. It keeps your digestive system moving, which is how your body clears out used-up estrogens so they don't recirculate and cause trouble.
Embrace Healthy Fats: Omega-3s—found in fatty fish like salmon, plus walnuts and chia seeds—are crucial for producing hormones and taming inflammation. Since chronic inflammation can scramble hormonal signals, keeping it low is a huge win. You can learn more by reading our guide on what inflammatory markers in blood work mean.
Consider Phytoestrogens: Certain foods like soy (think tofu and edamame), flaxseeds, and chickpeas contain plant-based compounds with a mild estrogen-like effect. For some women, especially during perimenopause, these can gently help smooth out the hormonal rollercoaster.
Master Stress and Prioritize Sleep
Chronic stress is one of the biggest hormone villains out there. When you’re constantly on edge, your body floods itself with cortisol, the main stress hormone. This can directly interfere with the production and balance of reproductive hormones like estradiol.
Your body is wired for survival, not necessarily for reproduction. High cortisol sends a loud and clear signal that it's a dangerous time, causing your system to down-regulate the hormones needed for a healthy cycle.
Building stress-resilience practices into your routine is essential to fight back. This doesn't have to be complicated—it could be mindfulness, a few deep breaths, yoga, or just a quiet walk outside.
Sleep is just as critical. Skimping on sleep also spikes cortisol and messes with the delicate hormonal regulation and repair work that happens overnight. Aim for a solid 7-9 hours of quality sleep each night. It's one of the most effective things you can do for your entire endocrine system.
When to Consider Medical Support
Lifestyle is your foundation, but sometimes it's not enough to solve the whole puzzle, particularly during major hormonal shifts like menopause. If symptoms of low or high estradiol are persistent and dragging down your quality of life, it's time to talk to your doctor.
For many women, options like Hormone Replacement Therapy (HRT) can be incredibly effective for managing menopausal symptoms by restoring declining estradiol levels. This is a very personal choice, one that should be made with a clinician who understands your health history and what you want to achieve. For a deeper look at wellness and hormone support, you might check out Anti-Aging Associates.
Ultimately, the best approach is a smart combination of informed lifestyle habits and expert medical guidance. That’s your most reliable path to finding and maintaining hormonal balance.
A Few Common Questions Answered
Hormones can feel complicated, but getting clear answers shouldn't be. Let's tackle some of the most common questions that come up about estradiol.
Can I Test My Estradiol Levels at Home?
You've probably seen ads for at-home hormone kits that use saliva or a finger prick. While they offer convenience, they often lack the precision needed for a hormone as dynamic as estradiol. For a truly accurate read, a serum blood test from a lab is still the best way to go.
A healthcare professional can then interpret that result in the context of other crucial hormones (like FSH) and your personal symptoms. This comprehensive view is essential for getting a reliable picture of what's really going on.
Will My Birth Control Pill Affect My Estradiol Test Results?
Yes, it absolutely will. Hormonal contraceptives like the pill, patch, or ring work by delivering synthetic hormones that deliberately suppress your body's own production of estradiol and progesterone.
If you test your estradiol while on hormonal birth control, the results will show very low levels of your natural estradiol, not your baseline. It's critical to tell your doctor about any and all medications you’re taking before you head to the lab.
The key takeaway here is that hormonal birth control essentially puts your natural cycle on pause. Testing estradiol levels in women who are using these methods won't tell you anything meaningful about your underlying ovarian function or natural hormone status.
What’s the Difference Between Estradiol and Estrogen?
This is a great question and a common point of confusion. The easiest way to think about it is that "estrogen" is the family name for a whole group of related hormones.
Estradiol (E2) is simply the most potent and prevalent member of that family during your reproductive years. The other two major players are estrone (E1), which takes over as the primary estrogen after menopause, and estriol (E3), the main estrogen during pregnancy. So, when you hear someone talking about "estrogen levels," they are almost always referring to estradiol because it's the one doing most of the heavy lifting.
At Outlive Biology, we transform your personal biometrics into clinical outcomes. By integrating data from wearables and comprehensive lab panels, our clinicians provide continuous monitoring and guidance tailored to your unique physiology, helping you optimize hormones, metabolism, and longevity. Take control of your health data today.

Live better for longer.
Research-backed tools, tactics, and techniques to maximize your health, delivered to your inbox every Monday.
Because real transformation starts with trust
and trust starts with clarity.
Founding Member Discount
Includes Devices + Labs
Cancel Anytime Before Activation