Longevity

Last Updated
Jan 2, 2026
A fasting insulin test measures how much insulin is circulating in your blood after you've gone without food for at least eight hours. It’s a simple blood draw, but the insight it provides is profound. This single number gives you a direct look at how hard your pancreas is working to keep your blood sugar in check, often revealing the first signs of metabolic stress long before it escalates.
Why Your Fasting Insulin Level Is a Critical Health Marker
Imagine insulin is the key that unlocks your cells, letting glucose—the energy from your food—get inside. When your metabolism is running smoothly, your pancreas makes just enough insulin to do the job. But what happens when the locks on your cells start to get a bit rusty and don't turn as easily?
That's the essence of insulin resistance. Your cells become less responsive to insulin's signal. To compensate, your pancreas has to pump out more and more of the hormone just to keep your blood sugar from rising. A fasting insulin test directly measures this extra effort, giving you a clear window into how efficiently your metabolic engine is running.
To give you a quick overview, here's a simple summary of what the test is all about.
Fasting Insulin Test at a Glance
Aspect | Description |
|---|---|
What It Is | A blood test that measures insulin levels after an 8+ hour fast. |
Primary Purpose | To assess insulin sensitivity and detect early signs of insulin resistance. |
Why It's Important | Provides an early warning for metabolic dysfunction, often years before blood sugar levels rise. |
Key Insight | Reveals how much insulin your body needs to maintain normal blood sugar, indicating metabolic efficiency. |
This table captures the core idea: it's not just about blood sugar, but the effort required to manage it.
An Early Warning System for Your Health
Standard check-ups usually focus on fasting glucose or HbA1c. While these are important, they're lagging indicators. They often only start to look problematic after your body has already been battling insulin resistance for years, sometimes even a decade.
The fasting insulin test is different. It's a proactive measurement that catches the underlying strain on your system much sooner. It helps you see the subtle metabolic shifts happening behind the scenes, giving you the power to make changes before prediabetes or type 2 diabetes ever become part of your story.
A Cornerstone of Modern Metabolic Science
Since insulin’s discovery back in 1921—a moment that turned a fatal diabetes diagnosis into a manageable condition—our understanding has grown immensely. The development of the fasting insulin test gave clinicians a tool to not only manage treatment but to diagnose insulin resistance, which has become a massive global health issue.
Understanding what causes insulin spikes is key to appreciating why keeping fasting insulin low is so fundamental to your long-term health. At Outlive Biology, we see it as an essential piece of the puzzle, which is why we incorporate it into a comprehensive panel of https://outlive.bio/biometrics to build a truly complete and actionable picture of your health.
How to Interpret Your Fasting Insulin Test Results
So, you've got your lab report back. That's the first step, but the real power comes from understanding what those numbers actually mean for your metabolic health. A fasting insulin test result isn't just a number on a page; it's a direct window into how well your body is managing its energy.
It's tempting to look for a simple "normal" or "abnormal" flag, but insulin levels are a spectrum. Think of it like the volume knob on a stereo. Your body might be keeping your blood sugar in a normal range, but to do so, it could be cranking the insulin volume to a deafening, unsustainable level. Just because you can hear the music doesn't mean it’s set right.
This decision tree can help you see why a fasting insulin test is such a valuable tool, whether you're feeling great or already dealing with symptoms.
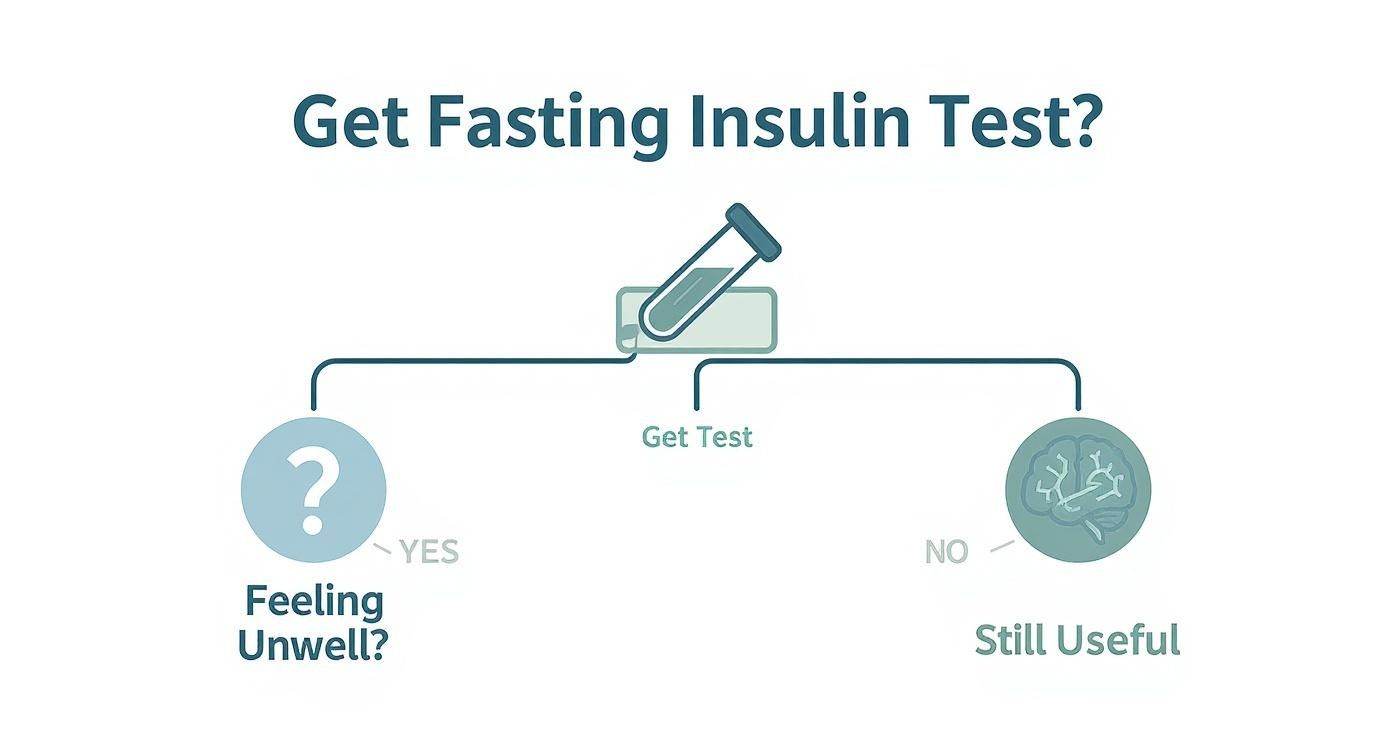
The big takeaway here is that this test isn't just for diagnosing problems—it’s one of the best proactive measures you can take for your long-term health.
Breaking Down the Numbers
Standard lab reports often have frustratingly broad "normal" ranges, sometimes flagging anything under 25 µU/mL as acceptable. From a preventive health and longevity standpoint, that’s not nearly specific enough. Our goal isn't just to be "not sick"; it's to be truly thriving.
Here’s a more functional way to look at your fasting insulin levels:
Optimal (Excellent Insulin Sensitivity): Below 5 µU/mL. This is the gold standard. It means your cells are listening carefully to insulin’s signals, and your pancreas isn’t working overtime.
Suboptimal (Early Insulin Resistance): Between 5 and 10 µU/mL. Many conventional labs would call this "normal," but it's a yellow flag. It suggests the first whispers of insulin resistance are beginning.
Concerning (Moderate Insulin Resistance): Between 10 and 20 µU/mL. Now, your body is working noticeably harder to keep blood sugar in check. This is a clear signal that metabolic dysfunction is taking hold.
High Risk (Significant Insulin Resistance): Above 20 µU/mL. Levels this high indicate a serious metabolic burden. Your risk for developing prediabetes, type 2 diabetes, and other chronic conditions is substantially elevated.
Looking at your results through these tiers helps you move beyond a simple pass/fail grade and see exactly where you stand on the metabolic health spectrum.
The Power of HOMA-IR
To get an even sharper picture of what's going on, we need to look at your fasting insulin in context with your fasting glucose. The calculation that does this is called the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR). It's a powerful score that shows the relationship between these two crucial markers.
The formula is pretty simple:
(Fasting Insulin in µU/mL) x (Fasting Glucose in mg/dL) / 405
Let’s walk through a quick example. Say your fasting insulin is 12 µU/mL and your fasting glucose is 95 mg/dL. Your HOMA-IR score would be:
(12 x 95) / 405 = 2.81
This score adds another critical layer of insight. An optimal HOMA-IR is generally considered below 1.5. A score between 1.5 and 2.5 points to early insulin resistance, while anything above 2.5 signals significant insulin resistance. In our example, a 2.81 is a clear sign of a metabolic issue that needs to be addressed.
The table below pulls these guidelines together, helping you translate your lab values into actionable knowledge.
Interpreting Fasting Insulin and HOMA-IR Levels
This table summarizes what the different ranges for both fasting insulin and HOMA-IR mean for your metabolic health, giving you a comprehensive snapshot.
Metric | Optimal Range | Suboptimal / Early Insulin Resistance | High / Significant Insulin Resistance |
|---|---|---|---|
Fasting Insulin | < 5 µU/mL | 5 - 10 µU/mL | > 10 µU/mL |
HOMA-IR Score | < 1.5 | 1.5 - 2.5 | > 2.5 |
What It Means | Your cells are highly sensitive to insulin; your metabolic system is efficient and running smoothly. | Your body is beginning to work harder to control blood sugar; this is an early warning sign. | Your pancreas is overproducing insulin to compensate for resistant cells; risk for metabolic disease is high. |
By looking at both your raw fasting insulin number and your HOMA-IR score, you can have a much more informed conversation with your doctor and get a real sense of where you need to focus. At Outlive Biology, we integrate these data points directly into your live dashboard. We track them over time, so you can see exactly how your personalized plan is improving your metabolic function at a deep, cellular level.
How to Prepare for an Accurate Fasting Insulin Test

When you're trying to understand your metabolic health, getting a clean, accurate reading is everything. A skewed test result can be more misleading than no test at all. The entire point of a fasting insulin test is to see what your body is doing at its baseline, without the noise from a recent meal or other variables. So, following the right prep protocol isn't just a suggestion—it's essential.
The most important rule is the fast itself. You’ll need to avoid all food and drinks, except for plain water, for a solid 8 to 12 hours before your blood is drawn. That means no morning coffee (not even black), no tea, and definitely no "harmless" additions like a squeeze of lemon or a zero-calorie sweetener. Even the smallest trigger can prompt an insulin release and throw off your numbers.
It’s More Than Just Not Eating
While avoiding food and drink is the foundation of a good fast, a few other, less obvious factors can also push your insulin levels around. Our hormonal systems are all interconnected, so things like a bad night's sleep, a stressful morning, or a tough workout can muddy the waters.
For example, just one poor night of sleep can tank insulin sensitivity by up to 30%. Hitting the gym for a high-intensity session right before your test can also temporarily change how your body handles glucose, affecting both your sugar and insulin readings.
To make sure your results are a true reflection of your metabolic state, stick to these simple guidelines:
Skip the Intense Workout: Hold off on any strenuous exercise for at least 24 hours before your test. A light walk is perfectly fine, but save the heavy lifting or intense cardio for another day.
Get a Good Night's Sleep: Do your best to get a full, restful night of sleep. This helps keep stress hormones like cortisol in check, which can directly interfere with your insulin levels.
Keep Your Morning Calm: A frantic, stressful morning can spike cortisol, which in turn can raise your blood sugar and insulin. Try to keep things as relaxed as possible on the way to your appointment.
Getting the Timing and Medications Right
When you schedule your test matters, too. Insulin has a natural daily rhythm, so the best practice is to have your blood drawn in the morning, usually between 8 and 10 AM, after fasting overnight. Sticking to this timing creates consistency, which is key for accurately tracking changes over time.
Finally, don't forget about medications and supplements. It’s crucial to have a conversation with your doctor about everything you’re taking before you go in for the test.
Make sure your provider knows about everything, including:
Prescription Drugs: Especially medications for diabetes, high blood pressure, or thyroid issues.
Over-the-Counter Medicines: Things you might not think twice about, like aspirin or allergy pills, can sometimes have an effect.
Vitamins and Supplements: Biotin is a well-known culprit for interfering with certain lab tests. For a deeper dive on this, check out our comprehensive guide to blood tests for vitamins and minerals.
By taking control of these variables, you’re no longer just guessing. You’re ensuring the number on that lab report is a true, reliable measure of your metabolic health. This is exactly the kind of high-quality data you and your team at Outlive Biology need to make the smartest decisions for your health journey.
Building the Full Picture with Glucose, HbA1c, and C-Peptide
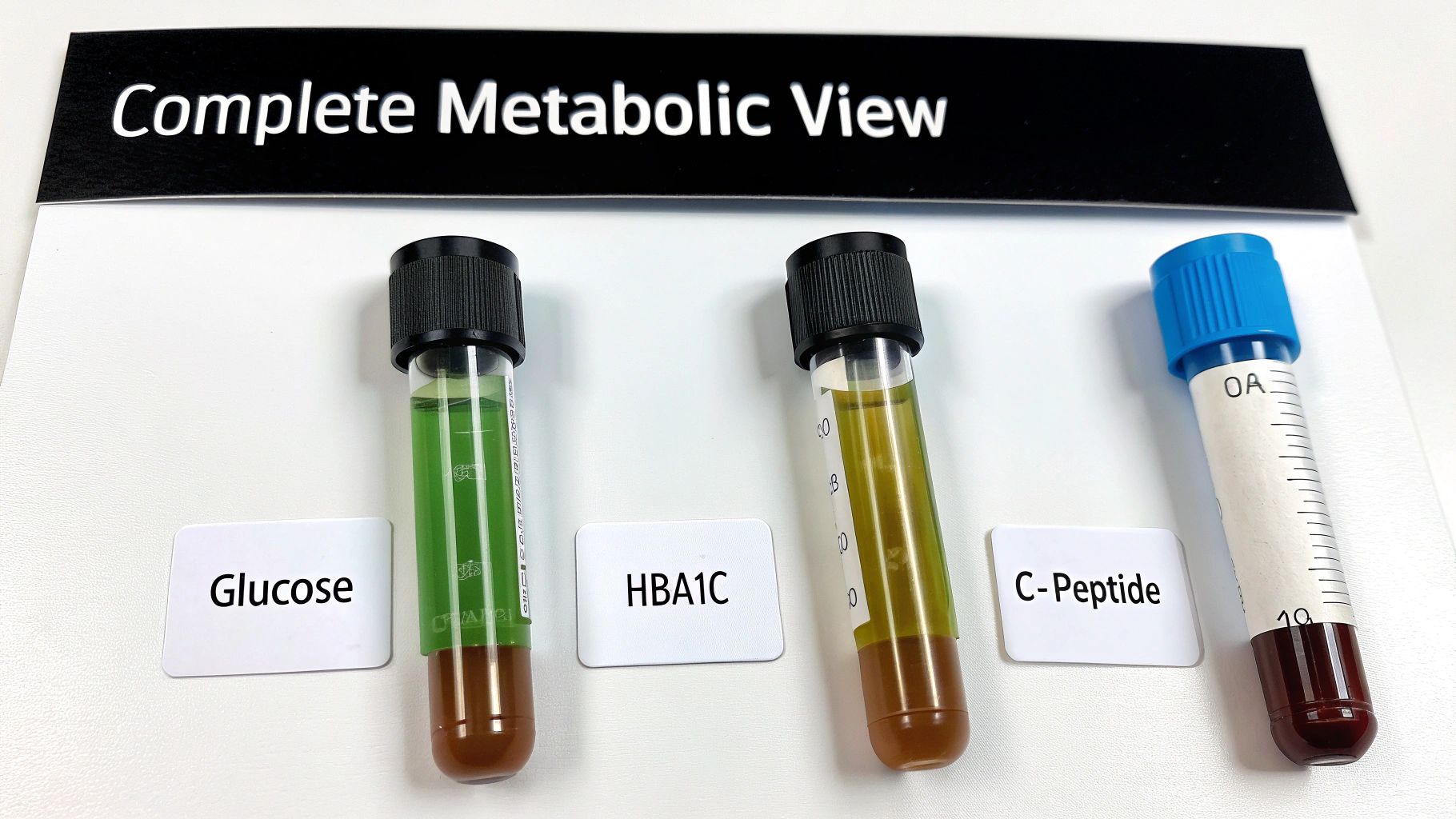
A fasting insulin test gives you a powerful, real-time snapshot of how much metabolic effort your body is exerting. But relying on this one data point is like trying to understand a movie by looking at a single frame. To truly grasp the plot of your metabolic health, you need to see how insulin interacts with the other key characters in the story.
By looking at your fasting insulin alongside biomarkers like fasting glucose, HbA1c, and C-peptide, we can build a much more detailed and dynamic picture of how your body manages energy. This lets us move past a simple reading and toward a deep understanding of your unique physiology.
The Immediate Snapshot: Fasting Glucose
Think of your fasting glucose as the speedometer in your car. It tells you exactly how much sugar is circulating in your bloodstream right now. While this is a critical piece of information, it can be misleading on its own. A normal glucose reading might look reassuring, but it doesn't tell you how hard your body's engine—your pancreas—is working to keep it there.
If your fasting insulin is high but your glucose is still in the optimal range, that's a classic sign of early insulin resistance. It means your body is successfully managing your blood sugar, but only by screaming at your cells with excessive insulin. This is a critical insight that a glucose test alone would completely miss.
The Long-Term Narrative: HbA1c
If fasting glucose is the speedometer, then Hemoglobin A1c (HbA1c) is the odometer's trip summary. It shows your average blood sugar levels over the past two to three months. This marker measures the percentage of your red blood cells that have become "glycated," or coated with sugar, giving you a stable, long-term view that isn't swayed by one bad meal or a stressful day.
An elevated HbA1c confirms that blood sugar control has been a persistent issue. When you see it alongside a high fasting insulin level, it paints a clear picture of chronic metabolic strain. It tells you not just that your body is working hard now, but that it has been struggling for a while.
The Factory Production Report: C-Peptide
Finally, there's C-peptide, which is perhaps the most direct partner to a fasting insulin test. When your pancreas produces insulin, it starts with an inactive form called proinsulin. This molecule is then split into two pieces: active insulin and a connecting fragment called C-peptide.
For every single molecule of insulin your pancreas makes, it also makes one molecule of C-peptide. This makes C-peptide an excellent proxy for your body's total insulin production—it's like getting a production report straight from the factory floor.
This is especially useful because C-peptide hangs around in the bloodstream longer than insulin, giving us a more stable measurement of pancreatic output. It helps answer a crucial question: is your high insulin level due to your pancreas overproducing it (a sign of early insulin resistance), or is something else going on?
To see how these markers work together, let’s look at a quick example.
Biomarker | Result | Interpretation |
|---|---|---|
Fasting Insulin | 15 µU/mL | High (indicating insulin resistance) |
Fasting Glucose | 95 mg/dL | Normal (body is still compensating) |
HbA1c | 5.5% | Pre-diabetic range (long-term strain) |
C-Peptide | High | Confirms pancreas is overproducing insulin |
In this scenario, all the pieces point to the same conclusion: significant, compensated insulin resistance that is just starting to impact long-term blood sugar control. Understanding the full story told by these markers is a core component of building a complete health picture, which is why they are often included in a comprehensive metabolic panel explained in depth by clinicians. At Outlive Biology, we analyze these interconnected data points to pinpoint the root cause of metabolic dysfunction and tailor interventions that address your specific needs.
Actionable Steps to Improve Insulin Sensitivity

Getting a high number back on your fasting insulin test isn't a life sentence—it's a starting line. Think of it as powerful data, a clear signal giving you a chance to take direct control over your metabolic health. Instead of feeling defeated, you now have the exact information needed to build a targeted and effective plan.
Forget vague advice like "eat better" or "move more." We're going to focus on specific, science-backed strategies that genuinely improve how your cells listen to insulin. We'll organize this around four key pillars: smart nutrition, effective exercise, restorative sleep, and proactive stress management. Each one is a critical piece of the puzzle, and when they work together, they can fundamentally shift your metabolic future.
Master Your Nutrition with Smart Choices
Improving insulin sensitivity doesn't mean waging a war on carbohydrates. It’s about being smarter with the quality, quantity, and timing of what you eat. The real goal is to give your body a steady stream of energy, not the sharp blood sugar spikes that send your pancreas into overdrive.
One of the best tools in your arsenal is fiber. Soluble fiber—the kind you find in oats, beans, avocados, and apples—acts like a sponge in your gut. It slows down sugar absorption, creating a much gentler energy curve and improving insulin sensitivity.
Meal timing matters, too. Adopting a consistent eating window, often called time-restricted eating, gives your digestive system a much-needed break. This allows your baseline insulin levels to fall and stay low for a good portion of the day, which can dramatically improve your cells' sensitivity over time.
Build a Powerful Exercise Routine
Physical activity is one of the fastest and most direct ways to improve insulin sensitivity. When you work out, your muscles act like glucose sponges, pulling sugar straight from your bloodstream for fuel—often without needing much insulin at all. The secret is finding a routine that mixes both cardio and resistance training for the biggest metabolic payoff.
Resistance training, like lifting weights or using bands, is especially powerful. Building more muscle gives your body more places to store glucose, which takes a huge load off your pancreas. Every pound of muscle is like a small fuel tank, ready to soak up excess sugar after you eat. Aim for two to three sessions a week, focusing on the big muscle groups.
Cardiovascular exercise is the perfect partner to strength training. Activities like brisk walking, cycling, or swimming don't just help your heart; they make your entire body more efficient at using glucose. It's a one-two punch:
Resistance Training: Builds the glucose "storage tanks" (your muscles).
Cardio: Improves the efficiency of your whole metabolic engine.
Prioritize Deep and Restorative Sleep
Sleep isn't a luxury; it's a non-negotiable pillar of metabolic health. Even one night of bad sleep can make you temporarily as insulin resistant as someone with prediabetes. It's during deep sleep that your body does its most critical maintenance work, including regulating the hormones that control your appetite, stress, and insulin response.
When you're chronically sleep-deprived, your body stays in a state of high alert, pumping out the stress hormone cortisol. Cortisol tells your body to release stored glucose, forcing your pancreas to produce even more insulin. This kicks off a vicious cycle: poor sleep raises insulin, and high insulin can wreck your sleep quality.
Make 7-9 hours of quality sleep a priority. The best way to do this is to set a consistent sleep schedule (even on weekends!), dim the lights in the evening, and put away screens before bed. Improving your sleep hygiene is one of the most effective levers you can pull to lower your fasting insulin. Since insulin is a key hormone, it's also worth understanding how to support your entire endocrine system. This guide on balancing hormones with supplements offers some great insights.
Actively Manage Your Stress Levels
Just like poor sleep, chronic stress keeps your cortisol levels sky-high. This hormone is in direct opposition to insulin. Cortisol wants to keep glucose readily available in your blood for a "fight or flight" scenario, while insulin wants to pack that glucose away into your cells. When these two are constantly at war, insulin resistance is almost inevitable.
This is why finding sustainable ways to manage stress is so crucial. You don't need to overhaul your entire life—it's about weaving small, consistent practices into your daily routine.
Here are a few proven methods that work:
Mindfulness and Meditation: Just 5-10 minutes a day can lower cortisol and calm your nervous system.
Breathing Exercises: Simple techniques like box breathing can immediately dial down your body's stress response.
Time in Nature: Getting outside has been scientifically shown to lower cortisol and boost well-being.
At Outlive Biology, we help you weave these strategies into a single, cohesive plan. By tracking your biometrics, we can see exactly how these changes are impacting your fasting insulin and other key markers. This allows us to fine-tune your approach in real-time for the best possible results.
Your Questions About the Fasting Insulin Test, Answered
Even with a solid grasp of the science, you're bound to have some practical questions when it's time to get a fasting insulin test. Let's walk through some of the most common ones so you can feel confident taking the next step in managing your metabolic health.
How Often Should I Get Tested?
The right testing schedule really depends on your starting point and your specific health goals. If your levels are already in a great spot (think below 5 µU/mL), checking in once a year during your annual physical is a smart way to make sure things stay on track.
On the other hand, if your results are in that suboptimal or high-risk zone, you'll want to check in more often. After you've started making changes to your diet, exercise, or sleep, your doctor will likely suggest retesting every three to six months. That's the sweet spot—it gives your body enough time to respond to the new habits and gives you valuable feedback on whether your plan is working or if it's time to tweak your approach.
Is This Test Covered by Insurance?
This is a big one, and the answer is: it depends. A fasting insulin test isn't always part of a standard check-up panel. Some insurance plans will only cover it if there's a specific medical reason documented, like a suspicion of insulin resistance or episodes of hypoglycemia.
Your best bet is to call your insurance provider directly and ask before you get the test. If it turns out it’s not covered, don't worry. The out-of-pocket cost is usually quite reasonable, and many people feel the insight it provides into their long-term health is a small price to pay for such powerful information.
What Is the Difference Between Insulin and Glucose?
It’s easy to get these two mixed up. Here’s a simple way to think about it: glucose is the fuel, and insulin is the key that lets the fuel into your cells.
Glucose is the simple sugar floating in your bloodstream, ready to be used by your cells for energy. It's the "what."
Insulin is the hormone that acts like a key, unlocking your cells so they can take in that glucose from the blood. It's the "how."
A glucose test measures how much fuel is circulating in your blood. A fasting insulin test, however, tells you how hard your body had to work—how much insulin it had to produce—to keep that blood glucose in a normal range. High insulin with normal glucose is a classic sign of a problem; it means your cells are becoming resistant to the key, and your body is overcompensating to get the job done.
At Outlive Biology, we believe that data is only as good as the action it inspires. We don’t just hand you your numbers; we help you understand the story they tell. By integrating your fasting insulin results with your complete health profile, we create a clear, personalized plan to improve your metabolic health for good.
Find out more about our data-driven approach at https://outlive.bio.

Live better for longer.
Research-backed tools, tactics, and techniques to maximize your health, delivered to your inbox every Monday.
Because real transformation starts with trust
and trust starts with clarity.
Founding Member Discount
Includes Devices + Labs
Cancel Anytime Before Activation