Hormones

Last Updated
Jan 2, 2026
The Free Androgen Index (FAI) is a calculated value that gives us a much better idea of how much testosterone is actually active and available for your body to use. Think of it less as a direct measurement and more as an insightful estimate of your true androgen status, going a step beyond just looking at your total testosterone number.
What the Free Androgen Index Actually Measures

Let's use an analogy. Imagine your total testosterone is all the money you have, including cash, stocks, and funds locked in a retirement account. The total amount looks great on paper, but it doesn't tell you how much cash you have on hand to spend right now. The Free Androgen Index is like your "disposable income"—it estimates the amount of testosterone that's free, unbound, and ready to get to work in your cells.
It's important to remember that FAI isn't a hormone itself. It's a ratio calculated from two other critical blood markers. This simple calculation cuts through the noise to reveal your level of bioavailable testosterone, the portion that truly influences everything from your energy and mood to your muscle mass and reproductive health.
The Two Key Players in FAI
To understand the FAI, you need to know about the two hormones it's based on: Total Testosterone and Sex Hormone-Binding Globulin (SHBG). They have a push-and-pull relationship that determines your androgen activity.
To give you a clearer picture, here’s a quick breakdown of what each component does and why it matters for the FAI calculation.
Key Components of the Free Androgen Index
Component | What It Is | Its Role in the FAI Calculation |
|---|---|---|
Total Testosterone | The total amount of testosterone in your bloodstream, including both "free" and "bound" forms. | This is the numerator—the starting point for figuring out how much testosterone is present overall. |
Sex Hormone-Binding Globulin (SHBG) | A protein that acts like a transport vehicle, binding tightly to sex hormones like testosterone. | This is the denominator—it represents the main factor that "locks up" testosterone, making it inactive. |
This table shows how the balance between your total supply of testosterone and the protein that binds it is what really counts.
Let's dive a bit deeper into these two components:
Total Testosterone: This is the big-picture number, representing every bit of testosterone circulating in your blood. It's a combination of the small fraction that's active (free) and the larger portion that's inactive (bound). For a deeper dive, check out our complete guide to understanding your testosterone levels.
Sex Hormone-Binding Globulin (SHBG): Think of SHBG as a fleet of hormonal taxis. Its main job is to latch onto sex hormones, including testosterone, and carry them through your bloodstream. The catch is, when testosterone is bound to SHBG, it’s essentially “occupied” and can’t interact with your cells to do its job.
Because SHBG holds onto testosterone so tightly, it keeps a large amount of it on the sidelines. This is why FAI is so useful. A high SHBG level can lock up a significant portion of your testosterone, which might lead to symptoms of low androgen activity even if your total testosterone seems perfectly normal. On the other hand, low SHBG means more testosterone is left free and active.
This insight is incredibly valuable in a clinical setting. For example, FAI has been widely studied as a key marker for androgen activity in women, particularly in relation to reproductive health and the changes that come with aging. A landmark longitudinal study on androgen changes followed hundreds of women through menopause and found that their FAI increased by an average of 16% in the decade before their final period, showing just how dynamic this marker can be.
Ultimately, by looking at the interplay between total testosterone and its primary binding protein, the free androgen index provides a much sharper and more clinically relevant picture of your body's hormonal environment.
Calculating and Interpreting Your FAI Score
So, how do we get to this Free Androgen Index score? It’s not something that’s measured directly in a blood sample. Instead, it’s a simple calculation that gives us a powerful snapshot of your hormonal landscape.
Think of it this way: your Total Testosterone is your entire supply, but SHBG is the protein that locks a lot of it up, keeping it inactive. The FAI calculation shows us the relationship between the two, revealing how much testosterone is actually free to do its job.
The formula itself is pretty straightforward:
For this to work, both your Total Testosterone and SHBG need to be measured in the same units—almost always nanomoles per liter (nmol/L). The result is a simple ratio, sometimes expressed as a percentage, that tells a much bigger story than either lab value on its own.
Putting the Formula into Practice
Let's make this real. Imagine a woman gets her lab work back and sees these two results:
Total Testosterone: 1.5 nmol/L
SHBG: 50 nmol/L
Plugging these into the formula, we get:
(1.5 / 50) x 100 = 3
Her FAI score is 3. But what does that number actually mean? On its own, not much. We need to compare it to established reference ranges to see if it’s in a healthy zone for her. In this case, a score of 3 is generally considered well within the normal range for an adult woman.
What Is a Normal FAI Score?
Here’s a critical point: "normal" FAI ranges can shift slightly depending on the lab doing the testing. Always check the reference range provided with your results.
That said, there are widely accepted guidelines that give us a solid frame of reference.
For adult women, the ranges typically look like this:
Normal Range: A score somewhere between 0.7 and 6.4 is usually a sign of a healthy androgen balance.
High Range: An FAI above 6.5 or 7.0 often suggests an excess of free, active testosterone. Scores climbing above 10 are a common finding in women with Polycystic Ovary Syndrome (PCOS).
Just for perspective, the typical FAI for an adult man is dramatically different, often falling somewhere between 30 and 150. This really underscores the natural hormonal differences between the sexes.
Understanding where you fall is key. A woman with an FAI of 8, for example, might finally have an explanation for symptoms like persistent acne or irregular cycles. A score of 2.5, on the other hand, sits comfortably in the typical female range.
This single number provides crucial context for other markers. When viewed alongside a comprehensive metabolic panel, it helps paint a much clearer picture of your overall metabolic and hormonal health.
Your FAI score translates a complex hormonal dance into one actionable number. Interpreted correctly, it’s a powerful tool that helps you and your doctor make truly informed decisions about your health.
How Normal FAI Ranges Change Through Life
Your Free Androgen Index (FAI) score isn’t a static number. To make any sense of it, you have to look at it in the context of your age, sex, and where you are in life. Think of it like blood pressure—what’s normal for a teenager is a world away from what’s normal for a senior citizen. Getting that context right is everything when it comes to interpreting your lab results.
The biggest divide, unsurprisingly, is between men and women. Men simply have far more total testosterone floating around, which means their FAI scores are often 10 to 20 times higher than women's. This is baseline physiology, and it’s why sex-specific reference ranges are non-negotiable.
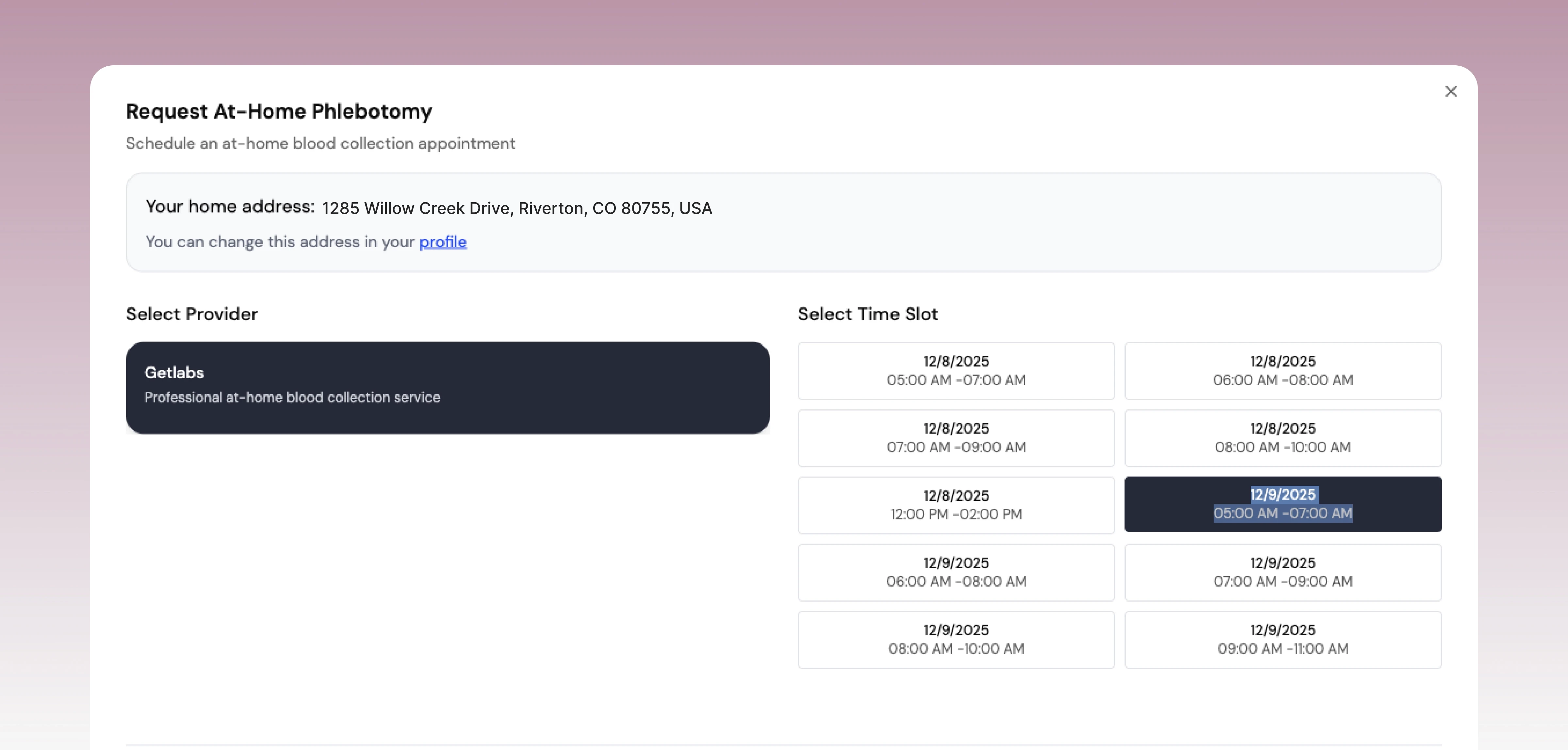
The infographic below really clarifies how this works. It breaks down the FAI calculation into its two core parts: Total Testosterone and SHBG. You can see how they work together to produce your final score.
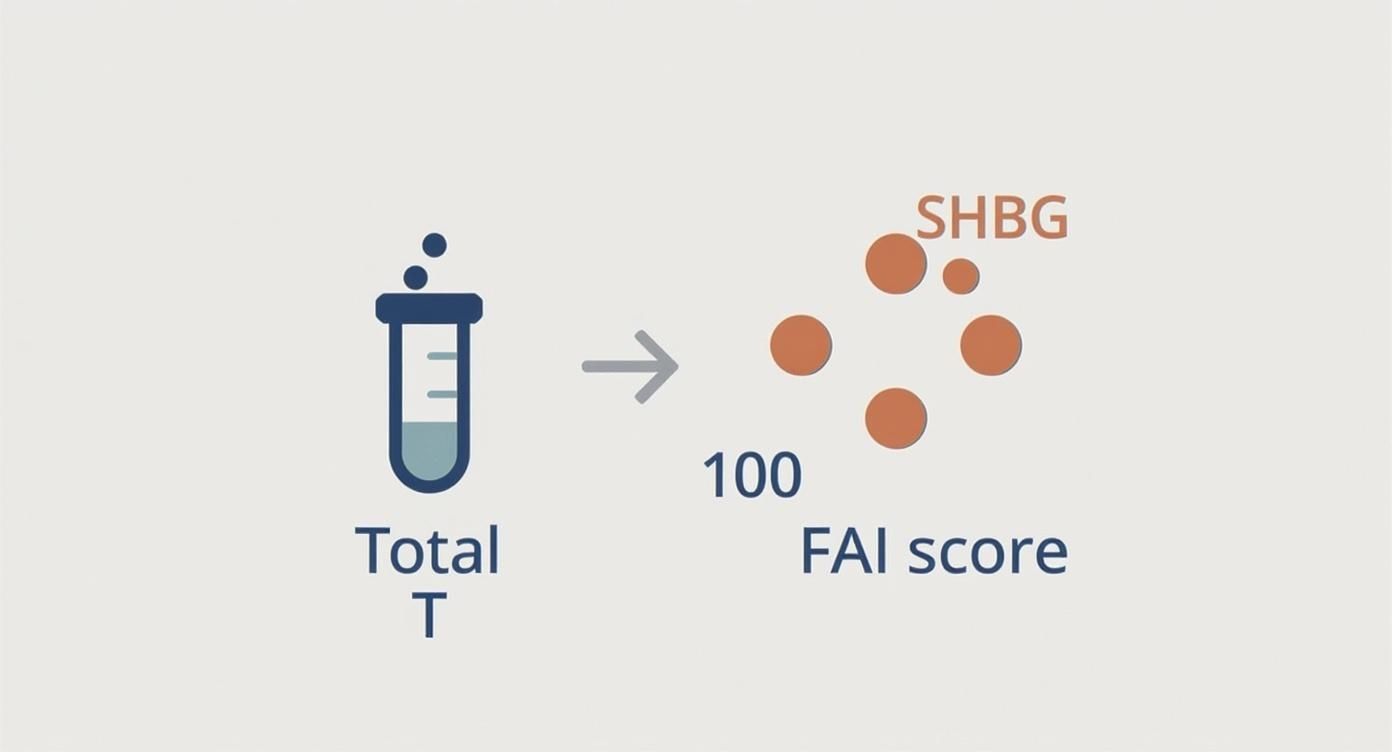
As the visual makes clear, a higher total testosterone or a lower SHBG will push your FAI up. On the flip side, lower testosterone or higher SHBG will pull it down.
Typical Free Androgen Index (FAI) Reference Ranges
To give you a clearer picture, here’s a table outlining some general FAI ranges. Remember, the exact numbers can vary a bit from one lab to another, so always compare your results to the reference range provided on your specific lab report.
Group | Typical FAI Range (Unitless Ratio) | Key Considerations |
|---|---|---|
Adult Women (Pre-menopause) | 0.5 - 7.0 | Levels can fluctuate with the menstrual cycle, pregnancy, and conditions like PCOS. |
Adult Women (Post-menopause) | 0.3 - 5.0 | SHBG often decreases, which can sometimes increase FAI even if total testosterone is falling. |
Adult Men (20-40 years) | 30 - 150 | Peak androgen activity; values are typically at their highest during this life stage. |
Adult Men (40+ years) | 20 - 100 | A gradual decline is expected as both testosterone production falls and SHBG levels rise. |
These ranges are benchmarks, not hard-and-fast rules. Your individual "optimal" number might sit anywhere within these zones, which is why tracking your personal trends over time provides the most valuable insight.
FAI Fluctuations in Women
For women, the FAI is an incredibly dynamic marker that ebbs and flows with major life events. These shifts are intimately tied to the hormonal rhythms that define a woman's reproductive journey.
A woman's FAI isn't a fixed point, but rather a moving target influenced by:
The Menstrual Cycle: While the changes are often subtle, androgen levels can shift throughout the month, frequently peaking around ovulation.
Pregnancy: To manage the massive surge in hormones, SHBG levels skyrocket during pregnancy. This usually causes the FAI to drop significantly.
Menopause: As the ovaries produce less estrogen, SHBG levels tend to fall. This can actually cause the FAI to rise, even if total testosterone is stable or declining, which alters the overall androgen balance.
Having solid reference ranges is critical here. For instance, a 2021 study set a reference range of 0.7–6.4 for women between 20 and 46. The research showed that healthy women in this group had an average FAI around 2.1±1.3, whereas women with PCOS—a condition linked to high androgens—had a much higher average of 4.4±3.8. You can dive deeper into how these numbers relate to conditions like hirsutism and PCOS by reading the original research.
The Gradual Decline in Men
In men, the story of the Free Androgen Index over a lifetime is usually one of slow, steady decline. This is driven by what’s sometimes called "andropause"—the natural, age-related drop in testosterone production.
It typically starts around age 30, when total testosterone begins to fall by about 1-2% per year. At the same time, SHBG levels often start to creep up. This one-two punch means the FAI score often drops more sharply than total testosterone alone, which can be linked to symptoms like low energy, reduced libido, and difficulty maintaining muscle mass.
Because these changes happen so gradually, tracking them over time is a game-changer. This is where a platform like Outlive Biology can be invaluable. By monitoring these subtle downward trends over months and years, you and your doctor can spot shifts long before they cause noticeable symptoms. This proactive approach allows for timely, data-driven decisions to help you maintain optimal androgen balance and feel your best as you age.
Understanding A High Free Androgen Index

When your lab report flags a high Free Androgen Index (FAI), it’s more than jargon—it means your body has too many free, active androgens, mainly testosterone. Clinicians call this hyperandrogenism, and it often shows up as real-world symptoms, not just numbers on a page.
An FAI above the normal range tells you one of two things (or both) is happening:
Your total testosterone is elevated
Your Sex Hormone–Binding Globulin (SHBG) is lower than it should be
The result? More unbound testosterone roaming free and influencing your cells, from skin to metabolism.
Polycystic Ovary Syndrome The Primary Culprit
In women, Polycystic Ovary Syndrome (PCOS) is the leading reason behind a raised FAI.
PCOS affects about 1 in 10 women of reproductive age.
It’s a top cause of fertility challenges.
Here’s why PCOS raises your FAI: the ovaries pump out extra androgens, throwing off the hormonal feedback loop that drives your menstrual cycle. Common signs include:
Hirsutism: Coarse, dark hair in male patterns—think face, chest, back.
Persistent Acne: Cystic breakouts around the jaw, chin, and neck that shrug off usual treatments.
Irregular Periods: Skipped or unpredictable cycles from disrupted ovulation.
Hair Thinning: Female-pattern loss at the crown and temples.
If acne is your battleground, you might explore natural approaches to treating hormonal acne as part of a wider strategy.
Other Causes Of A High FAI
While PCOS tops the list, a few other factors can push your FAI up:
Congenital Adrenal Hyperplasia (CAH): A genetic quirk making your adrenals overproduce androgens.
Ovarian or Adrenal Tumors: Rare, but some tumors secrete surplus androgens fast.
Medications: Anabolic steroids and certain drugs can spike testosterone levels.
Insulin Resistance: High insulin prompts ovaries to make more testosterone and cuts SHBG in the liver—a double whammy.
The Long-Term Health Risks Of A High FAI
Leaving high FAI unchecked isn’t just about unwanted hair or acne. It signals metabolic stress that can snowball into serious health issues.
Key risks include:
Type 2 Diabetes: Strongly linked to insulin resistance.
Cardiovascular Disease: Higher blood pressure and cholesterol imbalances.
Endometrial Cancer: Fewer periods lead to excessive endometrial growth.
Reproductive health also takes a hit. Studies show women with an FAI above 5 face a 68% miscarriage rate, compared to 40% for those within normal range. Discover more insights about these reproductive outcomes.
Whether you’re troubleshooting current symptoms or planning for future health, understanding and addressing a high Free Androgen Index is crucial. Continuous tracking—using services like Outlive Biology—helps you spot trends and tailor interventions over time.
What a Low Free Androgen Index Reveals
Just as a high score tells a story of excess, a low Free Androgen Index (FAI) paints an equally important picture of your hormonal health. When your FAI is low, it’s a strong signal that your body doesn't have enough active, bioavailable testosterone to do its job properly. This is often referred to as androgen deficiency.
Think of it this way: a low FAI score usually points to one of two problems under the hood. Either your body isn't producing enough total testosterone in the first place, or your SHBG levels are sky-high, grabbing onto testosterone and refusing to let it go.
Regardless of the cause, the end result is the same. There just isn't enough "free" testosterone available to interact with your cells, which can set off a chain reaction of noticeable and often frustrating symptoms.
For Men: A Telltale Sign of Hypogonadism
In men, a low Free Androgen Index is a classic indicator of hypogonadism—a clinical condition where the testes aren't producing adequate testosterone. This isn't simply a matter of getting older; it's a medical state that can seriously impact your quality of life.
Men with a low FAI often report a consistent set of issues:
Low Libido: A significant drop in sexual desire or interest.
Fatigue and Low Energy: A persistent feeling of being drained that sleep doesn't seem to fix.
Erectile Dysfunction: Trouble getting or maintaining an erection.
Loss of Muscle Mass: A frustrating decline in strength and muscle tone, even if you’re still hitting the gym.
Increased Body Fat: Especially stubborn fat around the midsection.
Mood Changes: Feeling more irritable, down, or just completely unmotivated.
The problem can originate from a couple of places. Primary hypogonadism means the issue is with the testes themselves, perhaps from an injury or a genetic condition. Secondary hypogonadism, however, traces back to the brain—specifically, the pituitary gland or hypothalamus aren't sending the right hormonal signals to kickstart testosterone production.
Low FAI in Women and Other Key Factors
While a high FAI is often the primary concern for women (think PCOS), a low score is far from meaningless. A low Free Androgen Index in women, particularly after menopause, can contribute to a general decline in well-being and vitality.
It's also important to remember that things other than age and sex can tank your FAI. Certain health conditions and medications are notorious for cranking up SHBG production, which effectively locks up your testosterone. This is where the FAI really shines—it can uncover an androgen deficiency even when your total testosterone levels look perfectly fine on paper.
Some of the biggest culprits that raise SHBG and lower your FAI include:
Oral Contraceptives: Birth control pills containing estrogen are well-known for dramatically increasing SHBG.
Liver Disease: Your liver is the SHBG factory, so conditions like cirrhosis can throw production out of whack.
Hyperthyroidism: An overactive thyroid gland can also cause SHBG levels to climb.
Extreme Weight Loss: Anorexia nervosa and other similar conditions disrupt the body's hormonal balance and can elevate SHBG.
Ultimately, understanding a low FAI is about connecting your lab results with how you actually feel. For both men and women, this number offers a vital clue into your body’s true androgen status, helping you and your doctor figure out the best path forward.
How to Proactively Manage Your Androgen Health
Your Free Androgen Index (FAI) score is a powerful piece of information, but it never tells the whole story on its own. True health management starts when you place that number into the bigger picture of your overall well-being and, with a professional, build a plan around it.
Think of your FAI as a single coordinate on a map. It shows you exactly where you are right now, but you need other data points to actually chart your course forward.
The first step is always to discuss your results with your doctor. They can look at your free androgen index alongside your symptoms, personal medical history, and other key lab tests. This 360-degree view is absolutely essential for getting an accurate diagnosis and creating a treatment plan that actually works.
When to Seek Clinical Guidance
Certain symptoms are red flags that it's time to have a conversation about your androgen levels. If you're dealing with any of the following, it’s a good idea to book that appointment.
For Women: Irregular menstrual cycles, adult acne that just won't quit, excessive hair growth (hirsutism), or unexplained challenges with fertility.
For Men: Nagging fatigue, low libido, erectile dysfunction, a noticeable loss of muscle mass, or significant shifts in your mood.
For Both: Unexplained weight gain or finding it nearly impossible to lose weight, especially if you have other hormonal symptoms.
These signs, especially when paired with an FAI that’s out of range, give your doctor a strong reason to dig deeper. For example, high androgens often go hand-in-hand with insulin resistance. Our guide to the fasting insulin test can help you understand this critical connection.
Strategies for Hormonal Balance
Once you have a clear clinical picture, you and your provider can start exploring strategies to support better androgen health. These can range from simple lifestyle adjustments to specific medical treatments, depending on whether your FAI is high or low.
For a high free androgen index, lifestyle changes are almost always the first line of attack:
Dietary Adjustments: Shifting to a whole-foods diet full of fiber and lean protein can do wonders for improving insulin sensitivity and supporting healthy SHBG levels.
Consistent Exercise: A smart mix of resistance training and cardio helps manage weight and fire up your metabolism.
If you have a low FAI, particularly for men diagnosed with hypogonadism, medical options might be on the table:
Every choice you make, from what you eat to the underwear you choose, can influence your hormonal environment. To get a sense of how even small daily habits can matter, it's worth understanding the science behind topics like boxers vs. briefs for fertility.
Ultimately, managing your androgen health is an ongoing process, not a one-and-done fix. Continuous monitoring with platforms like Outlive Biology gives you and your healthcare team the ability to track trends in your free androgen index over time. This lets you see what’s working, measure the real impact of your efforts, and make smart, data-driven adjustments to keep your plan perfectly tuned to your body.
Answering Your Top Questions About the Free Androgen Index
Even after digging into the details, you probably have a few specific questions about the Free Androgen Index and what it means for your health. Let's tackle some of the most common ones to give you a clearer picture.
Can FAI Help Diagnose PCOS?
Yes, a high Free Androgen Index is a major clue when diagnosing Polycystic Ovary Syndrome (PCOS). While it's not a silver bullet that diagnoses PCOS on its own, it’s powerful evidence of hyperandrogenism (excess androgens), which is a cornerstone of the condition.
Think of it this way: if a doctor sees symptoms like irregular periods and cysts on an ultrasound, a high FAI helps confirm that a hormonal imbalance is the engine driving those issues. It connects the dots between what you're feeling and what's happening with your hormones.
Does a High FAI Always Cause Infertility?
Not always, but it can certainly make getting pregnant a lot tougher. A high FAI is often a sign of the hormonal disruption that throws ovulation off track, and regular ovulation is non-negotiable for conception. When ovulation becomes unpredictable, the odds of conceiving naturally take a nosedive.
The good news is that many women with a high Free Androgen Index from PCOS go on to have successful pregnancies. This usually happens with medical guidance aimed at correcting the hormonal imbalance and getting ovulation back on a regular schedule.
Is It Possible for My FAI to Be Too Low?
Absolutely. We hear a lot about high FAI, especially in women, but a low FAI can signal its own set of problems. In men, a low Free Androgen Index is one of the classic signs of hypogonadism, which can lead to frustrating symptoms like chronic fatigue, low sex drive, and loss of muscle mass.
In women, a very low FAI can also drag down your overall sense of vitality, contributing to low energy and a lagging libido, particularly after menopause. This can happen if your body isn't producing enough testosterone, or more often, if your SHBG levels are sky-high due to things like oral contraceptives or certain liver conditions.
What Is the Difference Between FAI and Free Testosterone?
This is a fantastic and important question. The Free Androgen Index is a calculation—an estimate of your free, bioavailable testosterone based on your Total Testosterone and SHBG numbers. A direct Free Testosterone test, in contrast, is a lab measurement that tries to count the unbound testosterone molecules directly.
You might think a direct measurement is always better, but it’s a technically tricky test that can produce inconsistent results from lab to lab. Because of this, many doctors actually prefer using the FAI. It's reliable, affordable, and gives a clinically solid snapshot of your androgen activity based on two very accurate lab values.
Your health data tells a story, but you need the right tools to read it. Outlive Biology translates your blood labs, wearable data, and vitals into a clear, actionable plan for your long-term health. Stop guessing and start seeing your progress with continuous monitoring and expert guidance. Discover how data-driven care can optimize your androgen health at outlive.bio.

Live better for longer.
Research-backed tools, tactics, and techniques to maximize your health, delivered to your inbox every Monday.
Because real transformation starts with trust
and trust starts with clarity.
Founding Member Discount
Includes Devices + Labs
Cancel Anytime Before Activation