Blood Panels

Last Updated
Jan 2, 2026
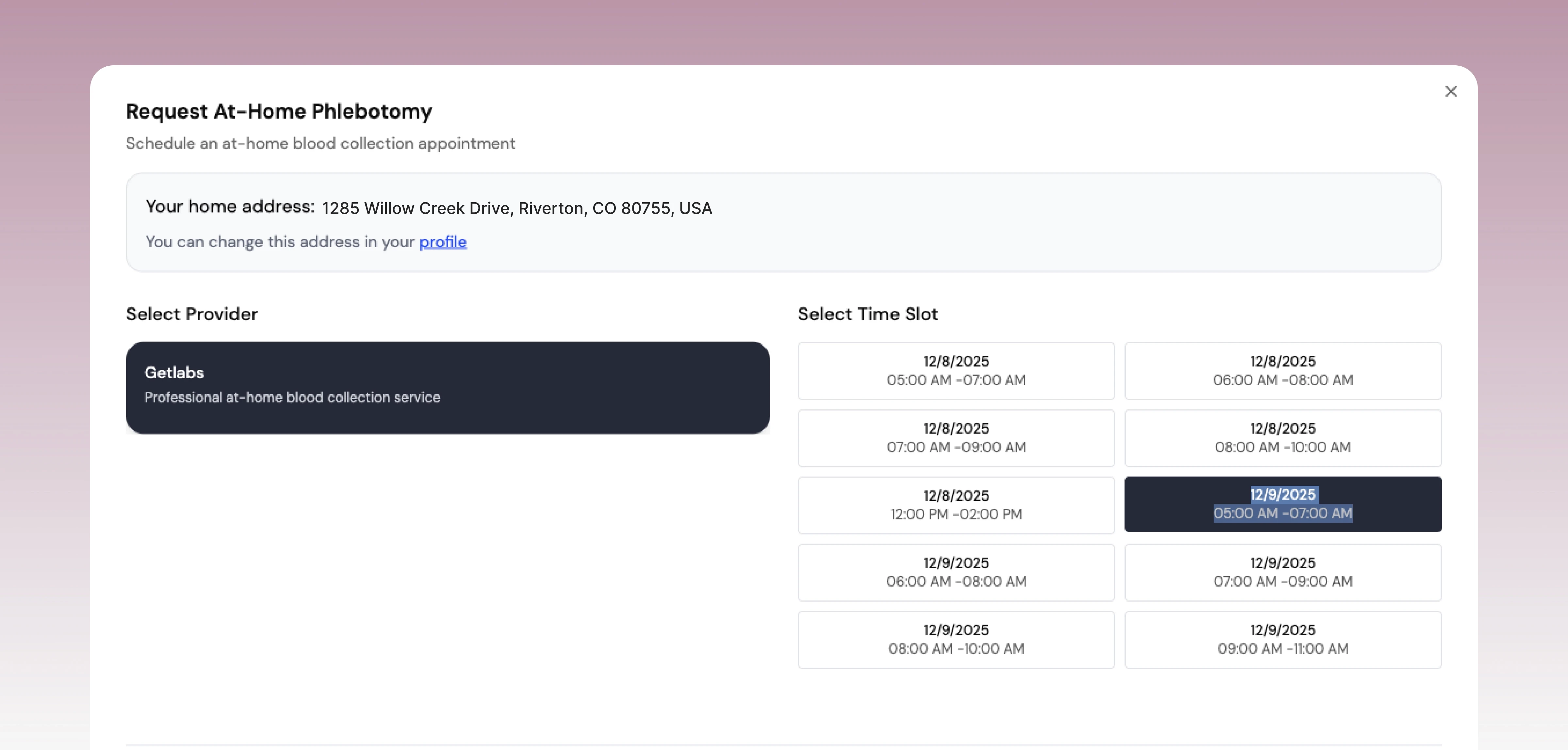
When you first get your blood work back, it's easy to feel overwhelmed. You're looking at a page full of acronyms and numbers, and it's not always clear what you should be focusing on.
The best way to start is by looking for three key things for each marker: its name, your result, and the lab's reference range. If your number falls outside that range, don't panic. It's simply the starting point for a conversation with your doctor to figure out what that result means for you, specifically.
Your First Look at Blood Work Results
Getting that lab report can feel like trying to crack a code. All those abbreviations and flags can be intimidating. But the basic layout is pretty straightforward. Each line item tells you what was measured, what your specific value is, and how that compares to a standard "normal" range.
Here’s the most important thing to understand right away: that reference range isn’t a universal standard for perfect health. It's just a statistical average, pulled from a huge group of people the lab assumes are healthy. This is a critical distinction—it means the range shows what's common, not necessarily what's optimal.
What Does the Reference Range Really Mean?
That "normal" range you see printed on the report represents the middle 95% of results from the reference population. The highest 2.5% and lowest 2.5% of values are automatically cut off. Because of this purely statistical method, 5% of totally healthy people will have results flagged as "abnormal" on any given test. Knowing this can help you look at your own numbers without jumping to conclusions. For a deeper dive, MedlinePlus has a great guide on how labs establish these ranges.
This is precisely why context is king. A number on a page means very little without the story behind it. So many things can nudge your results one way or another, including:
Your age and sex: Hormones, muscle mass, and even bone density markers naturally change as we get older.
What you ate and drank recently: Your diet and hydration levels in the 24 hours leading up to the test can temporarily shift everything from glucose and electrolytes to kidney function markers.
The time of day: Some hormones, like cortisol and testosterone, have natural daily rhythms and can be much higher or lower depending on when the blood was drawn.
A recent hard workout: Intense exercise can temporarily raise markers of inflammation and muscle damage, such as hs-CRP and creatine kinase.
The goal isn't just to be "within normal limits." It's about understanding your personal trends over time. A single lab test is a snapshot; tracking your results from one test to the next is what tells the real story of your health.
To help you get started, here's a quick cheat sheet for some of the most common acronyms you'll see on a report.
Key Blood Work Acronyms and What They Mean
This reference table can help you decode the most common abbreviations and terms found on your lab report.
Acronym | Full Name | What It Measures |
|---|---|---|
CBC | Complete Blood Count | Health of red blood cells, white blood cells, and platelets. |
CMP | Comprehensive Metabolic Panel | Kidney and liver function, electrolytes, blood sugar, and protein levels. |
BMP | Basic Metabolic Panel | A smaller version of the CMP, focusing on electrolytes and kidney function. |
HbA1c | Hemoglobin A1c | Average blood sugar levels over the past 2-3 months. |
hs-CRP | High-Sensitivity C-Reactive Protein | A marker for low-grade inflammation in the body, often related to heart health. |
TSH | Thyroid-Stimulating Hormone | How well the thyroid gland is functioning. |
LDL-C | Low-Density Lipoprotein Cholesterol | Often called "bad" cholesterol; a key marker for cardiovascular risk. |
HDL-C | High-Density Lipoprotein Cholesterol | Often called "good" cholesterol; helps remove excess cholesterol from the body. |
Having these terms down will make navigating your results a lot easier and help you pinpoint exactly what you want to discuss with your healthcare provider.
Moving from Normal to Optimal
This brings us to a more advanced way of reading your blood work: looking past the "normal" range to find your "optimal" range. The standard ranges are designed to flag outright disease. But an optimal range is typically much narrower and is focused on achieving peak health and longevity.
Take fasting glucose, for example. The standard lab range might go all the way up to 99 mg/dL. However, most clinicians specializing in longevity and preventive medicine prefer to see their patients consistently below 90 mg/dL to better minimize long-term health risks.
Approaching your results with this mindset empowers you to have a much more productive conversation with your doctor. You can move beyond asking, "Are my results normal?" and start asking, "Where do my numbers fall within an optimal range for someone with my specific health goals?" This simple shift in perspective turns your lab report from a passive document into an active roadmap for your health.
Decoding Your Complete Blood Count (CBC)
If there's a "workhorse" in the world of blood tests, it’s the Complete Blood Count, or CBC. It’s one of the most common labs a doctor will order, and for good reason—it gives a fantastic, high-level snapshot of your overall health.
Think of the CBC as a quick inventory of your body's most critical internal systems: oxygen transport and immune defense. It’s often the first place we look for clues related to infection, hidden inflammation, or anemia. Knowing what these markers mean can help you connect the dots between nagging symptoms like fatigue and what's actually happening in your biology.
Let's break down the key players.
Red Blood Cells: Your Oxygen Delivery Service
This section of your CBC tells the story of how well your body transports oxygen from your lungs to every single cell that needs it. If you’ve been feeling unusually drained, winded during light exercise, or just "off," the answers might be hiding right here.
When looking at your red cells, there are three main markers to pay attention to:
Red Blood Cell Count (RBC): This is exactly what it sounds like—the total number of red blood cells in your blood. A low count can mean you're losing them, destroying them, or simply not making enough.
Hemoglobin (Hgb): This is the crucial protein inside each red blood cell that actually grabs onto oxygen. Low hemoglobin is a classic sign of anemia.
Hematocrit (Hct): This number represents the percentage of your blood that's made up of red blood cells. It's a measure of concentration—are your red cells densely packed or a bit sparse?
I recently worked with a client who felt exhausted all the time, even with eight hours of sleep. His CBC flagged a low hemoglobin level. That single clue led us to check his iron and B12, and we quickly found a significant iron deficiency. With a few targeted dietary changes and the right supplement, his energy was back to normal in a matter of weeks.
A common misconception is that fatigue is just a normal part of a busy life. But if your RBC, hemoglobin, or hematocrit are low, it could be a clear sign of anemia—a treatable condition that's robbing you of your energy.
White Blood Cells: Your Immune System’s First Responders
Next up, we have the White Blood Cell (WBC) count. These are the soldiers of your immune system. Your total WBC count gives a general sense of immune activity—a high count often means your body is actively fighting something off, while a very low count might point to a weakened immune system.
The real gold, though, is in the WBC differential. This breaks down your white blood cells into their different types, each with a unique job:
Neutrophils: These are your front-line troops, the most numerous, and your primary defense against bacterial infections. A high neutrophil count is a strong indicator of an acute infection.
Lymphocytes: These are your specialists for fighting viruses and creating "memory cells" to prevent future infections. Elevated lymphocytes often point to a viral issue, like the flu or even just a common cold.
Monocytes: Think of these as the "clean-up crew," responsible for gobbling up dead cells and pathogens.
Eosinophils and Basophils: These are usually involved in allergic reactions and the response to parasites.
Seeing a shift in this differential can tell you so much. A sudden spike in neutrophils might finally explain why you feel so sick with what is likely a bacterial bug, while consistently high eosinophils could be the missing link to your seasonal allergies.
Platelets: The Clotting Crew
Finally, the CBC looks at your platelets. These aren't full cells but tiny fragments that are absolutely essential for blood clotting. Anytime you get a cut, platelets rush to the scene, stick together, and form a plug to stop the bleeding.
Having the right amount is key. If your platelet count is too low (thrombocytopenia), you might notice you bruise easily or have trouble stopping minor cuts from bleeding. On the flip side, if the count is too high (thrombocytosis), it could raise your risk of forming dangerous, unnecessary blood clots.
The CBC is a cornerstone of medicine worldwide because it provides so much data. A typical red blood cell (RBC) count, for example, is between 4.2 to 5.4 million cells/mcL for women and 4.7 to 6.1 million/mcL for men. Hemoglobin usually falls between 12 to 18 grams per deciliter, while platelet counts should sit between 150,000 to 450,000 per microliter. Clinicians rely on these standardized ranges to diagnose everything from anemia to infections. For a deeper dive, you can find more insights on CBC interpretation at CEUFast.com.
By understanding these three core components—red cells, white cells, and platelets—you can turn a confusing lab report into a powerful tool for understanding your own body.
Making Sense of Your Metabolic Panel
While the CBC gives you an inventory of your blood cells, the metabolic panel—often called a Comprehensive Metabolic Panel (CMP) or Basic Metabolic Panel (BMP)—is like peeking under the hood at your body’s engine. It’s a snapshot of your metabolism, kidney and liver function, electrolyte balance, and more.
Think of it as the real-time control panel for your body's chemistry. These markers are sensitive, shifting with everything from your last meal to your hydration levels. This makes them powerful, immediate indicators of your physiological state. Let’s walk through the key components so you know exactly what you’re looking at.
Glucose and Your Metabolic Health
The first number most people’s eyes jump to is glucose. This is a direct measurement of the sugar in your bloodstream at the moment the sample was taken. A fasting glucose test, done after an 8-12 hour fast, provides a clean baseline of how your body manages blood sugar without the immediate influence of food.
A high fasting glucose can be an early warning sign of insulin resistance, a condition where your cells become numb to insulin's signal to absorb sugar. Left unchecked, this can pave the way for prediabetes or type 2 diabetes. While a single high reading isn’t a diagnosis, it’s a clear signal to take a closer look at your diet, exercise, and stress.
It’s also crucial to remember that a lot of things can temporarily nudge your glucose up. A stressful morning, a poor night's sleep, or even just the "white coat" effect of being in a clinical setting can cause a spike. This is precisely why tracking these numbers over time gives you a much more accurate story than obsessing over a single result.
Electrolytes: The Body's Electrical System
Next up, we have the electrolytes—minerals that carry an electric charge and are absolutely vital for nerve signaling, muscle contractions, and hydration. The main players you'll see on a CMP are:
Sodium: The primary regulator of fluid balance and nerve impulses. Its levels are closely tied to your hydration status and kidney function.
Potassium: Essential for a steady heartbeat and proper muscle function. Both high and low levels can cause issues.
Chloride: Works hand-in-hand with sodium to maintain fluid balance and the body's acid-base (pH) levels.
An imbalance here can be the culprit behind symptoms like muscle cramps, fatigue, or even heart palpitations. For instance, after a really sweaty workout or a bout of stomach illness, you might see your sodium and potassium levels dip, which is your body telling you it's time to rehydrate and replenish those minerals.
Your metabolic panel is a dynamic snapshot. Unlike a genetic test, these markers can—and do—change based on your daily choices. This gives you direct, actionable feedback on how your lifestyle is impacting your internal health.
Kidney Function Markers
Your kidneys are your body’s master filtration system, tirelessly working to clear waste products from your blood. The CMP gives you two key indicators of how well they’re performing.
Blood Urea Nitrogen (BUN): This measures urea nitrogen, a waste product created when your body metabolizes protein.
Creatinine: This is another waste product, generated from the normal daily wear and tear of your muscles.
If BUN and creatinine are elevated, it could suggest your kidneys aren't filtering waste as efficiently as they should. But context is everything here. A high-protein diet or simple dehydration can temporarily raise BUN, while someone with a lot of muscle mass will naturally have a higher baseline creatinine. For a deeper dive on all the markers in this panel, check out our comprehensive metabolic panel explained guide.
Liver Enzymes: Indicators of Liver Stress
Finally, the CMP checks in on your liver health by measuring key enzymes, primarily Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST). These enzymes are supposed to live inside your liver cells.
When liver cells are damaged or inflamed, they start to leak these enzymes into your bloodstream, causing their levels to rise on a lab report. Elevated ALT and AST can be a sign of liver stress from many sources, including alcohol, certain medications, viral infections, or the increasingly common non-alcoholic fatty liver disease (NAFLD).
But here’s another crucial nuance: even a tough workout can cause a temporary, harmless spike in these enzymes. This is especially true for AST, which is also found in muscle cells. It's a perfect example of why you can't interpret these numbers in a vacuum. Always consider your results in the context of your recent activities and overall health.
Understanding Your Cholesterol and Lipid Panel
For decades, the conversation around cholesterol has been boiled down to a simple good-vs-bad story. But a lipid panel tells a much richer, more nuanced story about your cardiovascular health than just one "total cholesterol" number.
The real key is to see these numbers not as a final grade, but as dynamic feedback on your diet and lifestyle. They show you exactly how your choices are impacting your long-term heart health. Let's move past the outdated labels and dig into what these markers really mean for you.
Decoding the Key Lipid Markers
When you get your lipid panel back, you'll see a handful of primary measurements. Each one offers a unique piece of the cardiovascular puzzle, and understanding their individual roles is what helps you see the complete picture.
Here are the main players you need to know:
Low-Density Lipoprotein (LDL-C): Often called the "bad" cholesterol, LDL’s actual job is to deliver cholesterol from the liver to cells that need it. The trouble starts when you have too much LDL floating around. It can begin to build up in your artery walls, forming the plaque that hardens and narrows them—a process called atherosclerosis.
High-Density Lipoprotein (HDL-C): This is the "good" cholesterol, and for good reason. HDL acts like a cleanup crew, scavenging for excess cholesterol in your arteries and carrying it back to the liver for disposal. This is why higher levels are so protective.
Triglycerides: Think of these as the fat your body uses for immediate energy, found floating in your blood. High levels are a huge red flag, often tied directly to a diet high in sugar, refined carbs, and alcohol. They're a significant independent risk factor for heart disease.
Total Cholesterol: This is simply the sum of your LDL, HDL, and a few other lipid components. It's a useful number at a glance, but without the context of the individual parts, it doesn't tell you much.
Someone with a "normal" total cholesterol could still be at high risk if their HDL is in the tank and their triglycerides are through the roof. That's precisely why looking at the relationships between these numbers is so critical.
Why Ratios Matter More Than Single Numbers
More and more, clinicians are focusing on the ratios calculated from a lipid panel. Why? Because they often give a much sharper assessment of your risk than any single marker ever could. These ratios put your numbers into context, revealing the real balance between your protective and potentially harmful lipoproteins.
Two of the most insightful ratios are:
Triglyceride/HDL Ratio: This is an incredibly powerful predictor of insulin resistance and heart disease risk. A high ratio (you really want to see it below 2.0) suggests a pattern of small, dense LDL particles—the kind that are much more likely to create plaque.
Total Cholesterol/HDL Ratio: This ratio gives you a sense of your overall cholesterol load relative to your protective HDL levels. Lower is always better here, with an ideal target often sitting below 3.5.
Focusing on these ratios can completely shift your mindset. Instead of just trying to hammer down one "bad" number, you start working to improve the overall harmony of your metabolic health. It’s a far more complete and actionable way to see your results.
Turning Your Results into Action
Here's the most empowering part: your lipid panel is incredibly responsive to lifestyle changes. Unlike some genetic factors that feel out of your hands, you have a massive amount of control over these numbers.
I once worked with a member at Outlive Biology whose triglycerides were north of 250 mg/dL—well into the high-risk zone. Before even thinking about medication, we focused entirely on his diet. He committed to cutting out sugary sodas and dialing back his intake of processed snacks. In their place, he started eating whole foods rich in omega-3s, like salmon and walnuts.
The result? In just three months, his triglycerides dropped below 150 mg/dL, and his HDL cholesterol climbed by 10 points. His lab report went from being a source of anxiety to a source of motivation. He had tangible proof that his hard work was fundamentally changing his health from the inside out.
Here are a few practical steps you can take to move your own lipid panel in the right direction:
To lower LDL and Triglycerides: Slash your intake of refined carbohydrates, added sugars, and industrial trans fats. Amp up your soluble fiber from foods like oats, apples, beans, and psyllium husk.
To raise HDL: Get moving with regular, vigorous exercise. Prioritize healthy fats from sources like avocados, high-quality olive oil, and nuts.
By learning to read the nuances of your lipid panel, you can transform a simple blood test from a confusing report card into a personalized roadmap for better cardiovascular health and a longer, healthier life.
What to Do After You Get Your Results
Your lab report isn't the finish line—it's the starting gun. When you get that document filled with numbers and flags, it’s easy to feel like that’s the final word. But the real value is in what you do next. The whole point is to turn that passive data into an active strategy for your health, starting with a much better conversation with your doctor.
Instead of just asking, "Is this normal?" you can walk into your appointment ready to dig deeper. This proactive approach ensures you get the most out of your visit and leave with a clear, actionable game plan.
Prepare for Your Doctor's Appointment
Walking into your doctor's office with your results and a list of targeted questions is a game-changer. It shifts the dynamic from a simple review to a collaborative strategy session about your health. A little prep work goes a long way.
Before your visit, try this:
Review and Highlight: Go through your report and circle anything flagged as high or low. But don't stop there. Highlight any markers you're curious about, even if they're technically "in range."
Connect to Your Symptoms: Think about how you've been feeling lately. Is your energy dragging? Sleep a mess? Jot down any symptoms next to the relevant markers. For example, you might write "Feeling tired all the time" next to your hemoglobin result.
Note Your Lifestyle: Make a few notes about your diet, exercise, stress levels, and sleep in the week leading up to the test. This context is gold. A couple of tough workouts or a high-stress week at work can absolutely influence your results.
This simple preparation helps your doctor see the whole picture. It allows them to connect the lab data to your real-world experience, leading to a much more personalized and effective plan.
Track Your Results Over Time
One of the biggest mistakes I see people make is treating a single blood test as the definitive verdict on their health. It’s not. A single test is just a snapshot in time. The real insights come from tracking your results over multiple tests to spot the trends. This is where you can truly understand what the numbers mean for your own body.
A single high glucose reading might be a fluke caused by a bad night's sleep. But a pattern of steadily rising glucose over three consecutive tests? That tells a much more urgent story about your metabolic health.
When you track your labs, you establish your personal baseline. This helps you and your clinician distinguish a temporary blip from a meaningful change that needs attention. This is a core principle at Outlive Biology, where we analyze serial labs to create protocols that adapt as your own data evolves.
Learn the Language of Your Labs
Getting comfortable with the specific units and abbreviations on your report is key. Globally, labs use standardized units to ensure consistency. For instance, you'll see mg/dL (milligrams per deciliter) for things like glucose and cholesterol, while enzyme activity is often measured in IU/L (international units per liter).
One critical red blood cell metric, Mean Corpuscular Volume (MCV), is measured in femtoliters (fL). The normal range is typically 80-100 fL, and a value outside this can point to specific types of anemia. If you want to dive deeper, you can explore a comprehensive guide on blood test results to understand what these globally accepted units signify.
Here’s a simple visual to help you start connecting the dots on your lipid panel.
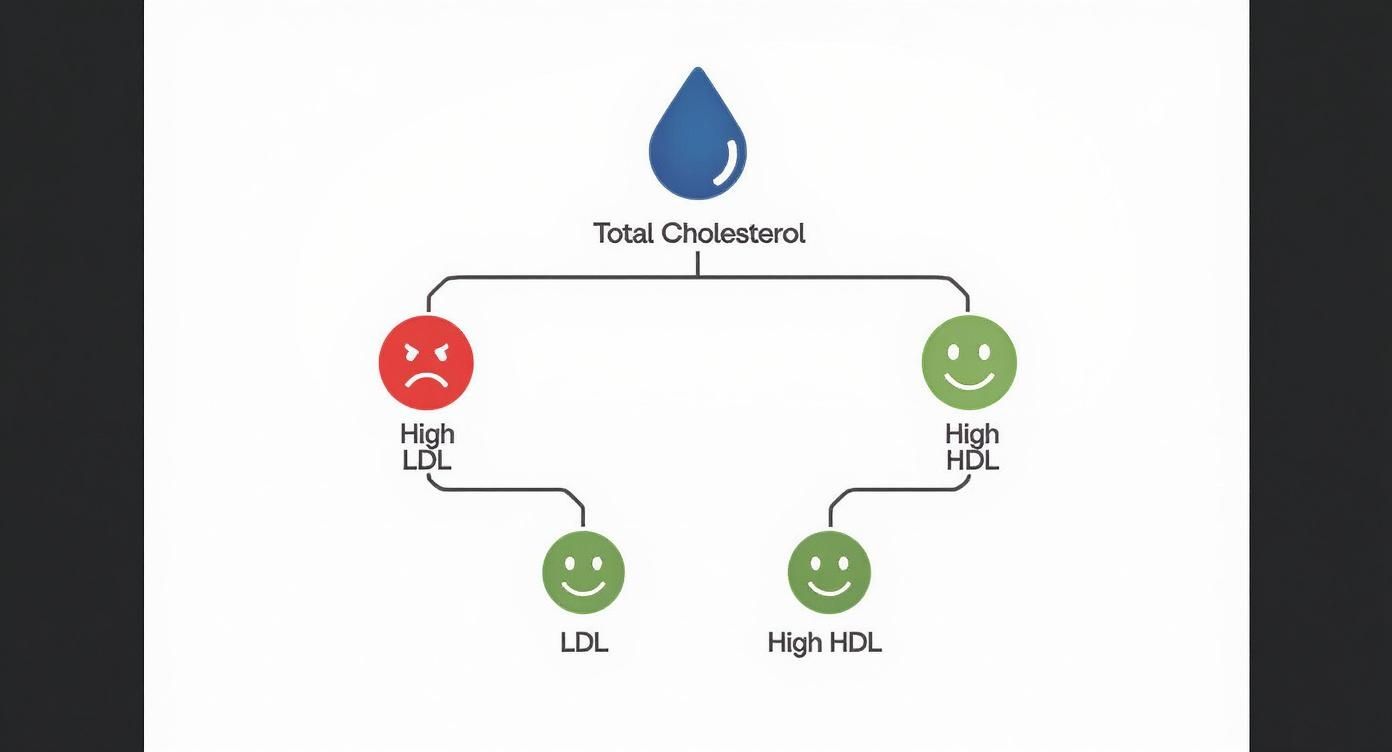
This chart breaks down the main components of your total cholesterol, showing why high LDL is a concern while high HDL is generally a good thing for your heart health.
Take Action with Lifestyle Adjustments
Finally, the most empowering step is connecting your results to things you can actually do. Think of your lab report as direct feedback on how your daily habits are impacting your internal biology. Seeing a number in black and white can be the ultimate motivation to make a change.
The following table provides a quick look at how certain results can point toward specific lifestyle adjustments.
Common Blood Markers and Lifestyle Influences
Blood Marker | Potential Meaning of High/Low Result | Actionable Lifestyle/Dietary Steps |
|---|---|---|
Fasting Glucose | High: Potential insulin resistance or pre-diabetes. | Reduce intake of added sugars and refined carbs. Increase fiber, protein, and healthy fats. |
ALT/AST (Liver Enzymes) | High: Indicates potential liver stress or inflammation. | Reduce or eliminate alcohol. Limit processed foods and high-fructose corn syrup. |
Triglycerides | High: Linked to diet high in carbs/sugar, excess alcohol. | Focus on omega-3 fatty acids (fish, flax), limit refined carbs, and incorporate regular exercise. |
hs-CRP (Inflammation) | High: General systemic inflammation. | Anti-inflammatory diet (leafy greens, berries), manage stress, prioritize sleep. |
Vitamin D | Low: Insufficient sun exposure or dietary intake. | Get sensible sun exposure. Consider supplementation with D3, especially in winter. |
HDL Cholesterol | Low: Increased cardiovascular risk. | Increase regular aerobic exercise. Consume healthy fats like avocado, nuts, and olive oil. |
This isn't an exhaustive list, of course, but it shows how direct the line can be from a number on a page to a choice you make at your next meal or a decision to go for a walk.
By taking these steps, your blood work transforms from a confusing medical document into your own personalized roadmap. It becomes an indispensable tool for managing your health, preventing problems down the road, and simply feeling your best every single day.
Common Questions About Blood Work
Getting your lab results back often sparks more questions than it answers. Once you have a handle on the main panels, you start wondering about the practical stuff—how often should I really be getting tested? What does it mean if my glucose is just a tiny bit high? Let's dive into some of those common questions with some real-world, practical advice.
Knowing how to prep for a blood draw or what to do with a borderline result is just as crucial as understanding the markers themselves. This is all about feeling confident in the process, from the day before your appointment to the conversation you have with your doctor afterward.
What Should I Do If My Result Is Just Outside the Normal Range?
It’s easy to feel a jolt of anxiety when you see a result flagged as “high” or “low,” but a single marker that’s barely outside the standard range is rarely a cause for immediate panic. Remember, your body is a dynamic, living system, not a static piece of machinery.
Fluctuations are completely normal. All sorts of things can temporarily nudge a marker one way or another:
Fighting off a cold or minor infection
A killer workout the day before your test
Not drinking enough water or what you had for dinner
A particularly stressful week at work
So, what's the first step? Don't jump to worst-case scenarios. The best move is to discuss it with your healthcare provider. They're trained to see that one number in the context of your entire health picture—your other lab values, how you're feeling, and your overall history. More often than not, the plan is simply to re-test that marker in a few weeks to see if it was just a blip or if it’s part of a developing trend we need to watch.
How Often Should I Get My Blood Work Done?
There’s no magic number here; the right testing frequency is deeply personal. It really depends on your age, your current health, and what you’re trying to achieve.
For a generally healthy adult with no major health issues, getting a comprehensive panel done every one to two years is a solid baseline for preventative care. That cadence shifts dramatically, however, if you're managing a specific condition. For instance, someone with a thyroid disorder or diabetes might need labs every three to six months to make sure their treatment plan is working effectively. And if you’re proactively working on optimizing your health, you might choose to test more often to see how your lifestyle experiments are impacting your key biomarkers.
How Can I Prepare for a Blood Test to Get Accurate Results?
Good preparation is everything. If you don't prep correctly, you're not getting a true snapshot of your baseline health. The golden rule is to always follow the specific instructions given by your doctor, since different tests have different needs.
For instance, any test that requires fasting—like a lipid panel or fasting glucose—means no food or drinks (other than water) for a solid 8 to 12 hours beforehand. It's also a good idea to skip any intense exercise and alcohol for at least 24 hours before your draw, as both can skew markers related to liver function and inflammation. Staying hydrated with plain water is a must, too; being dehydrated can artificially bump up values like hematocrit and certain kidney markers. Gaining a deeper understanding of what are inflammatory markers in blood work can shed more light on how your daily habits influence these numbers.
A pro tip: Always tell the phlebotomist about every medication and supplement you're taking. Something as common as biotin, for example, can throw off the results of certain hormone assays. Full transparency is the only way to get a truly accurate reading.
At Outlive Biology, we see your health data as an ongoing dialogue, not just a static report card. We take these numbers and weave them into a personalized action plan, combining your lab results with real-time data from wearables to build a complete, dynamic picture of your health. See how we turn biometrics into better health outcomes at https://outlive.bio.

Live better for longer.
Research-backed tools, tactics, and techniques to maximize your health, delivered to your inbox every Monday.
Because real transformation starts with trust
and trust starts with clarity.
Founding Member Discount
Includes Devices + Labs
Cancel Anytime Before Activation